Download and print as a PDF (574kB pdf)
On this page
- What is this information about?
- Why have I been given this information?
- What is an abdominal drain?
- Why do I need a drain?
- Will I feel any pain from the drain?
- Will I go home with the drain in?
- What do I need to do at home?
- When and how should I measure the drainage (fluid)?
- What should I do if I have any problems with the drain?
- How long will I need the drain for?
- How will the drain be removed?
- Changing the drainage bottle: step-by-step instructions
What is this information about?
This information is about having an abdominal drain. It explains what an abdominal drain does, why you need one, and what happens if you go home with a drain. It also includes:
- a chart to record the fluid coming out of your drain.
- a guide to changing the bottle on your drain if you need to.
- what to do if you experience any problems.
- a chart to record any follow-up notes and discussions with your nurse.
Why have I been given this information?
You have been given this information because it is important that you know how to take care of yourself, and your drain, when you leave hospital and go back home. If you need to change your drainage bottle, following the instructions in this leaflet will help you to do this safely.
It is also important that you keep a record of the fluid that comes out of your drain. You can keep track of this on the drain chart included here.
What is an abdominal drain?
A drain is a tube with many holes at the end, which is placed in the abdomen, or close to the area surgery took place inside the body.
The abdomen, or abdominal cavity, is the space inside your body which contains organs including the stomach, liver, pancreas, spleen and kidneys.
The drain is added here to remove fluid that may collected after an operation. The end of the tube that comes out of your body will be attached to a bag or bottle which is either:
- fastened to your leg with straps, or
- shortened, and the end placed inside a bag attached to your stomach.
You may need to carry the bottle-style drains around.
Why do I need a drain?
When body tissues (like muscles or skin) are cut during an operation, fluid will leak out afterwards.
A leakage of fluid in a closed cavity (space) can cause pain and possibly infection.
This leakage might be a lot, or it might be a kind of fluid that can cause problems to your health. Because of this, it is helpful to drain it outside of the abdominal cavity.
This will help with healing; reduce pain and discomfort; and reduce the risk of internal infections.
Will I feel any pain from the drain?
You may feel discomfort around the drain site.
You may also get discomfort or pain internally (inside you) where it rubs against tissues and organs. For example, after gallbladder surgery the drain may sit under the liver and cause pain or discomfort, particularly when you move.
Please take painkillers to ease this. It is important to continue moving to avoid other post-operative complications such as chest infections and deep vein thrombosis (blood clots).
Will I go home with the drain in?
If you are well and do not need to be in hospital but still need a drain, you may leave hospital and go home with the drain still in. This is not unusual and there is no need to worry. The nurse looking after you will show you how to care for the drain and give you the supplies needed.
There are different options to look after your drain:
- If you are unable to get out of the house once you get home, a district nurse may visit you at home to support you with the drain and monitor the skin around the drain.
- If you can leave the house, then the practice nurse at your GP surgery can offer this support.
- You can monitor the drain site and change the bags or bottles yourself if you feel confident to do so. You can discuss this with the nurse on when you leave hospital.
There are instructions below about looking after the drain.
What do I need to do at home?
If at any time you need to check the drain site, change the bag, bottle or dressings, wash your hands thoroughly before and after with soap and water and a clean towel.
You will be shown how to attach clean bags or bottles before discharge. There are step-by-step instructions below if you chose to do this at home.
Be careful not to get the drain caught on any furniture to prevent it being pulled out.
Keep the drain lower than the wound to allow drainage to continue.
When and how should I measure the drainage (fluid)?
You should measure the drainage at roughly the same time each day or when the bag or bottle is two-thirds full, whichever is sooner. Please see the chart below.
It is important to note the colour of the fluid coming out as this indicates what may be draining. For example, green if it is bile, red if it is blood or yellow if it is tissue fluid. It is important to keep track of the volume of fluid from your drain so you can recognise what is normal output for you and when something isn’t right. This will also help us to know when the drain can be removed.
- Empty the fluid in the bag or bottle into the jug supplied (the nurse will show you how before you leave hospital).
- Note the amount in millilitres and the colour of the fluid.
- Write this on the chart supplied.
If you have more than one drain you need a separate chart for each drain.
What should I do if I have any problems with the drain?
If you have any problems, please do not worry, contact the number supplied.
- If the stitch holding the drain in place comes loose, secure with a dressing if possible. You will have been given this by your nurse before you leave hospital. Please contact the hospital on the number you have been given to arrange a time to come in and have the stitch replaced.
- If the drain falls out, place a piece of gauze or clean dressing over the site. You will have been given this by your nurse before you leave hospital. Please contact the hospital to make them aware so they can decide if the drain needs to be replaced.
- If the fluid coming out of the drain drastically increases, contact the number provided.
- If you feel unwell or have a high temperature, call the nurse, your GP, or if severe come to A&E.
- If you have lots of fluid leaking from the area where the drain comes out, cover with gauze or a fresh dressing. You will have been given this by your nurse before you leave hospital. Please contact the hospital so they can decide if you need to be reviewed face to face.
- If you notice any signs of infection around the drain site, please ring us or see your GP as you may need antibiotics.
Signs of infection include:
- increased swelling
- redness
- yellow or green pus (this is usually cloudy fluid)
- a bad smell
- increased pain around the drain site
How long will I need the drain for?
This will depend on the type of surgery you have had and your individual circumstances.
It will also depend on the amount of fluid draining and the type of fluid.
How will the drain be removed?
The drain will be removed after consultation with the surgical team. The nurse will discuss the plan with you, so you know what to expect.
When you come for your appointment to get the drain removed, it is a good idea to take some painkillers (like paracetamol) before you attend.
The stitch holding the drain in place will be cut and the drain slowly pulled out. The area will then be dressed, or a small wound bag applied over the site. This may continue to leak a small amount of fluid afterwards.
You will be supplied with some spare dressings or bags to apply at home.
If you need any help after the drain has been removed, you could ring the ward you were discharged from for advice, or the contact number you may have been given.
For a drain chart, please see the PDF version of this leaflet at the top of the page.
Changing the drainage bottle: step-by-step instructions
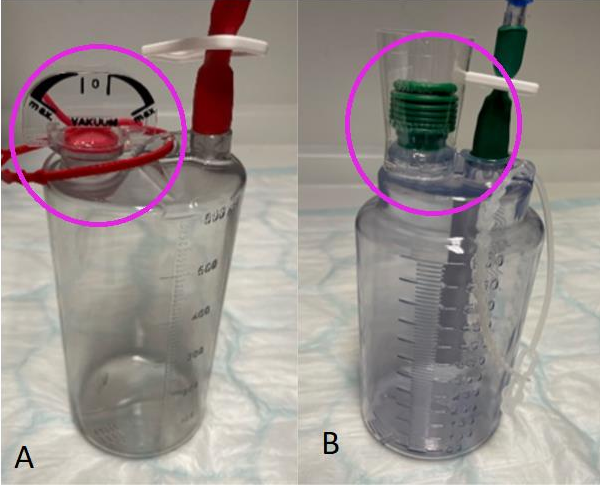
Please see the above picture of vacuum drain bottles. If you have this type of drain this is
how they should look when they are working correctly.
Picture (A) and (B): see circled areas.
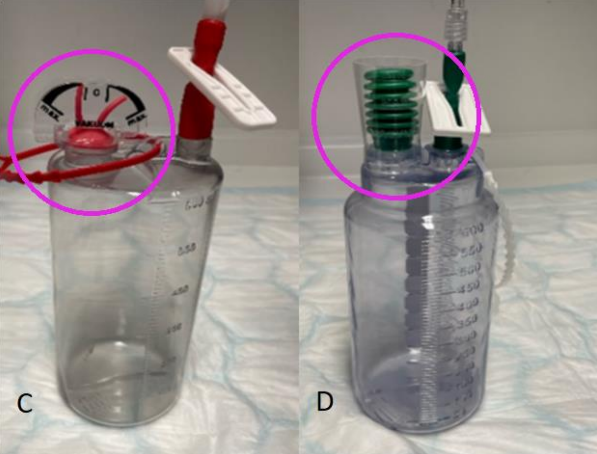
You may need to change the bottle at home if the bottle is full, if the tubing has disconnected
or the suction has been lost.
Picture (C) and (D) above show each drain when they have lost their suction: see circled
areas.
Changing your drainage bottle:
The steps below give instructions on how to change your bottle at home, if necessary. A nurse will demonstrate this for you before you are discharged from hospital.
1. Wash your hands thoroughly with soap and water. Close the clip on the tubing of the bottle to be changed:

2. Close the clip on the bottle to be changed:

3. Disconnect the tube from the bottle by unscrewing the luer lock (connector).
4. Screw on the new bottle. Make sure it is on tightly as loose connections can lead to a loss of suction:

5. Open the clip on the tubing:

6. Open the clip on the bottle:

For ‘Follow up notes’, see the PDF version of this leaflet at the top of the page.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.