Download and print as a PDF (342kB pdf)
On this page
- What is superficial keratectomy?
- What is alcohol delamination?
- Why is the procedure done?
- What is the benefit of having this procedure?
- What are the possible risks following surgery?
- What happens on the day of surgery?
- What should I expect after the surgery?
- Who should I speak to for further information and advice?
What is superficial keratectomy?
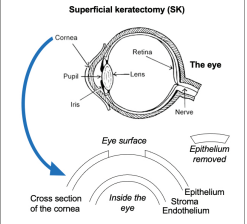
Superficial keratectomy (SK) involves the removal of the front layer of the transparent window of your eye or cornea, leaving the middle and deeper layers intact. This layer is called the epithelium, and like skin cells, the corneal epithelial cells shed and regenerate every couple of days.
What is alcohol delamination?
This procedure is assisted by applying alcohol to the eye’s surface. This loosens the attachment of the surface epithelial cells, making them easier to remove.
Why is the procedure done?
This procedure is performed when the corneal surface has become irregular or roughened, e.g. due to surface scarring. This can also be performed in recurrent corneal erosion syndrome (RCES).
RCES affects the cornea’s outer surface layer (the eye’s clear front window). The surface becomes unstable and breaks down to form an erosion or raw area, exposing the nerves beneath the surface. This can occur due to an injury, e.g. a scratch to the eye or some corneal dystrophy like Map Dot Fingerprint Dystrophy.
What is the benefit of having this procedure?
Depending on the reason the procedure is performed, it may help in reducing recurrent erosions and providing comfort. It may also help to improve your vision. The procedure’s benefits will be evident in 2 to 4 weeks (corneal smoothing) or over the next few months if the aim has been to prevent recurrent corneal erosions.
What are the possible risks following surgery?
• Infection of the cornea.
• Corneal opacity (cloudiness).
• Delayed or failure of healing of corneal surface (epithelium).
• Recurrent corneal erosions.
What happens on the day of surgery?
These procedures are usually carried out as a day-case procedure. Typically only local anaesthetic is required by using eyedrops to numb the eye. The procedure usually takes under 30 minutes to perform, although this may vary between patients. At the end of the surgery, a bandage contact lens may be placed on the eye, or the eye may be padded closed with antibiotic ointment.
What should I expect after the surgery?
After the operation, you will have a sore and painful eye for the first few days. This is because it can take 2 to 5 days for the scratch from surgery to heal.
You will be provided with local anaesthetic eyedrops to ease the pain, and you will receive clear instructions on how to use them. Always use them per the prescribed limits, as excessive use of these drops can result in delayed healing and further complications such as infection. You can also take over-the-counter painkillers as needed.
You will be given antibiotics and steroid eyedrops after the operation, generally about four times a day for two weeks.
You will have a post operative check up a few weeks after surgery. This is to ensure the cornea has healed well and to remove the bandage contact lens if one has been used. Sometimes, the lens falls out on its own; if this happens, you should discard it.
Driving: the legal requirement for driving is to read (with glasses or contact lenses, if necessary) a number plate at 20 metres, with both eyes open. You may be able to meet this requirement a few days after surgery, but if you are unsure of if you rely on your operated eye for driving acuity (perception), please ask for advice at your follow up appointment.
Work: it is likely to be challenging to work for the first few days to a week. Please ask your doctor should you require a sick note.
Who should I speak to for further information and advice?
If you have problems or need urgent advice, ring the eye hospital. Ask for the Accident and Emergency Department (A and E) or Nursing Staff. There is always someone on duty, night and day.
Sussex Eye Hospital, Eastern Road, Brighton BN2 5BF
Out of Hours telephone
01273 664881
Compiled by: Ms Ritika Mukhija, MBBS, MD, FRCOphth. Dr Gabriella Quiney, MBBS and Mr Mayank A. Nanavaty, MBBS, DO, FRCOphth, PhD.
This leaflet is intended for patients receiving care in Brighton and Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.