Download and print as a PDF (724kB pdf)
On this page
- Who will look after me during my hospital stay?
- What is a broken hip?
- How will the doctors fix my hip?
- What operation will I have if the break is across the neck of the thigh bone?
- What operation will I have if the break occurs below the neck of the thigh bone?
- What are the risks of having a broken hip and of the surgery to fix it?
- What will happen to me before the operation?
- What will happen to me after my operation?
- Rehabilitation after surgery
- How will I get back on my feet?
- How long will I be in hospital?
- What happens when I leave hospital?
- Will I recover completely once my broken hip has been repaired?
- How can I reduce my risk of an injury in the future?
- Useful contact numbers
Who will look after me during my hospital stay?
A multidisciplinary team of healthcare professionals will look after you during your hospital stay. The team includes:
Surgical orthopaedic consultant
This is the senior surgeon who is responsible for your care in the days near your operation.
Medical orthogeriatric consultant
This is the senior medical doctor who is also responsible for your care. They look at your medical problems and review the tablets which you need. They will continue to care for you once the surgeon is happy with the results of your operation.
Anaesthetic consultant
This is the senior medical doctor who will give you an anaesthetic for your operation.
Junior doctors
A team of orthopaedic doctors will work with your consultants and will see you most days.
Ward nursing staff
A team of nurses who care for you on a day to day basis.
Discharge liaison nurse
A nurse specialist who may work with you and your family to help ensure a safe and timely discharge from hospital.
Physiotherapists (Physios)
Physiotherapists will work with you to progress your mobility until you are safe to be discharged home, or your mobility has reached a point where it has stopped improving.
Occupational therapists (OTs)
Occupational therapists assess your abilities and needs with everyday tasks, such as washing, dressing or preparing a meal.
Social worker
The social worker helps to advise and organise any continuing care needs you may have when you are discharged from hospital.
Dietician
The dietician may assess your diet and nutritional requirements.
Other health care professional
There are many other professionals who we may ask to assist with your care if you have particular a medical condition.
What is a broken hip?
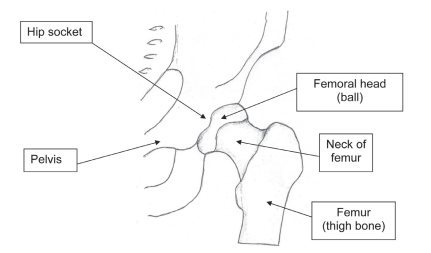
The hip joint is a ball and socket joint between your pelvis and thigh bone (femur). A broken hip, sometimes called a ‘hip fracture’ or ‘fractured neck of femur’, describes a range of fractures of the thigh bone near the hip joint.
How will the doctors fix my hip?
A broken hip is a common injury in later life. Having an operation to fix the hip will give you the best chance of walking again and recovering from the injury.
More than 98% of hip fractures need surgery before patients can walk again. About 77,000 hip fractures are fixed by surgery each year in the UK. In Brighton we operate on more than 500 patients with a broken hip each year. Two main types of hip fracture occur. The break can be across the neck of the thigh bone or can be below the neck of the thigh bone. Each requires a different type of operation.
What operation will I have if the break is across the neck of the thigh bone?
There are two types of hip replacement for a break across the neck of the thigh bone. A ‘half hip replacement’ and a ‘full or total hip replacement’.
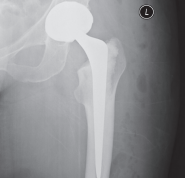
- Hemiarthroplasty (‘half a hip replacement’). If the break occurs across the neck of the thigh bone, then the blood supply to the head of the thigh bone may be damaged, and the head will not heal. In this case, the surgeon will remove the head and replace it with a metal ball and stem which fits into the top end of the thigh bone. This operation is known as a ‘hemiarthroplasty’ or ‘half a hip replacement’.
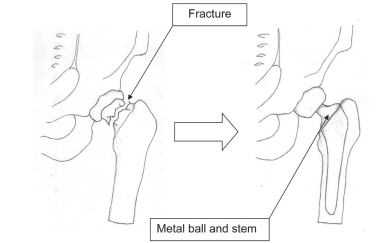
2. Total hip replacement. This is like a half hip but the ‘socket’ is also replaced. This operation is usually done in patients who could walk with minimal assistance outdoors before the injury and who will have a good understanding of the rehabilitation process.
What operation will I have if the break occurs below the neck of the thigh bone?
Dynamic hip screw (‘DHS’). If the break has occurred lower down then the blood supply to the head of the thigh bone is not damaged. In this case, a metal screw and plate system is used to hold the edges of the bone together while they heal naturally.
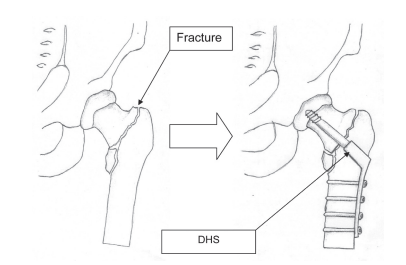
In all cases, the metalwork will stay in the hip forever, unless there is a specific reason to remove it. The length of the scar that remains after surgery varies according to the type of metalwork inserted, but usually varies between 4 inches (10cm) and 12 inches (30cm). Although you may be away from the ward for a number of hours the operation usually takes about 75 minutes to perform.
What are the risks of having a broken hip and of the surgery to fix it?
Risks related to having a broken hip
A hip fracture is a very serious injury and can be life threatening in some cases. Some patients do not survive the hospital admission and some decline in the months following discharge. The fracture in itself is a sign that you are vulnerable and that your health may deteriorate in the short or longer term.
Common problems are
Confusion: worsening memory is very common following a broken hip. Often it improves over time but in some cases the deterioration is permanent.
Chest infection: worsening mobility puts you at risk of developing a chest infection or pneumonia.
Clot in the leg: worsening mobility puts you at risk of a thrombosis or clot in the leg which can move to the lungs and make you very unwell.
Fall in hospital: most hip fracture patients have many risk factors for falls. Being in an unfamiliar hospital environment with a painful weak leg increases this risk further.
Diarrhoea: some of the medication can upset your bowels. Antibiotics make clostridium difficile diarrhoea more likely. Occasionally hospitals experience an outbreak of the seasonal diarrhoea and vomiting bugs.
Pressure sores: many patients have fragile skin. Reduced mobility and poor nutrition puts you at increased risk of a sore especially on your bottom or heels.
Risks related to the surgery: without an operation you will be unable to walk, you will have significant pain and the problems outlined on the previous page will all be much more likely. We therefore almost always recommend an operation, however there are risks associated with this also.
Wound infection: this can be a leaking wound for a few days which settles with antibiotics. About 2 patients in 100 can develop a deep infection in the metal work. This can require further surgery and a prolonged hospital admission. This is one of the most serious complications.
Dislocation: a half or full hip replacement metal ball can move out of the socket. This is known as a dislocated hip. This is an uncommon problem. If it does happen then an operation to put the hip back is usually needed. If the problem recurs then the hip metal work may need changing.
Failure of fixation: this is also uncommon. The hip screw can move in the bone into an abnormal position over time. If this happens then further surgery may be needed.
A further break: the thigh bone can occasionally crack during the surgery. This can delay your return to walking by many weeks. If you fall on the repaired leg then the thigh bone can break again below the metalwork.
At Haywards Heath, we use a computer database to keep a very close eye on complications, so that we can carry on reducing the risks of them happening in future.
What will happen to me before the operation?
You will be admitted by the nursing staff on the ward. Routine assessments of your falls risk whilst in hospital, nutrition and pressure care will all be completed.
You will meet the surgical team. Before your operation, the surgeon will explain to you what type of break you have, and what type of operation would provide the best fix.
The surgeon will mark the skin over your broken hip with a pen before surgery, and will ask for your permission to perform the operation. You will be asked to sign a consent form. The surgeon can speak to your relatives if you wish.
In order to get you ready for surgery, to make you comfortable and in a good fit state for the operation, the surgical team will arrange the following for you:
- Painkillers. Regular painkilling tablets will be prescribed. If you are in pain, ask the nurses for extra painkillers.
- Intravenous fluids (a ‘drip’) You are not allowed to eat or drink for several hours before surgery. You will be given fluids into the veins to stop you getting dehydrated.
- Blood clot prevention. This will involve wearing elastic stockings and having small, daily injections under the skin for about a month after the operation.
- Blood tests and scans You might need more tests in addition to the ones you had in the Accident and Emergency department.
- A catheter. If you find it too difficult or uncomfortable to use a bed pan, the nurse might fit you with a plastic tube to drain your urine .
You will meet the Anaesthetic Team. Before your operation you will be visited by an anaesthetist. There are two main types of anaesthetic used. You will be advised which is the most suitable for you.
- General anaesthesia. This is where drugs are given that make you sleep during the operation. Local anaesthetic injections to the groin or lower back may be offered to you, to provide additional pain relief. These relieve the pain for 4 to 6 hours after the operation.
- Regional (‘spinal’) anaesthesia. After receiving some sedative drugs to make you feel sleepy, you will be given a small injection in the middle of the lower back which will numb your body below the belly button during and after surgery (for several hours). You do not sleep with this type of anaesthetic, which allows you to recover quicker after the operation. In Brighton 80% of operations happen within the first 2 days of the admission. Your operations may be delayed if you require other treatment or tests, or if there is an increased demand on the hospital for emergency surgery. We will keep you and your family informed about any delays.
What will happen to me after my operation?
When you leave the operating theatre, you will be taken to a recovery area in the theatre suite, where you will be looked after by a special nurse until you come round from your anaesthetic / sedation. The nurse will check that you are warm and comfortable, and that your blood pressure and heart rate are normal, before you are taken back to your ward bed.
You may feel sick or groggy for several hours after the operation. Drugs can be given to stop you feeling sick.
With the break fixed, you should feel more comfortable. A nurse will check your pain level regularly, and will give you painkillers if you need them.
All patients lose some blood during a hip operation. Depending on your blood tests and general health, you may need a blood transfusion before, during or (more commonly) after your operation.
Constipation is common after a hip operation. Ask your nurse for laxatives (bowel medicine) if you are having trouble opening your bowels.
You may feel confused after the operation. Usually this is mild and gets better by itself, but your doctor may need to do further tests or give more treatment if you become very confused.
You will be encouraged to build up your strength after the operation by eating regularly. Additional ‘build-up’ drinks may be given to you if you are having difficulty swallowing more solid food.
You will be seen after your operation by the physiotherapist, who will show you some deep breathing exercises and help you get up and out of bed if you are well enough. This helps to reduce the risk of chest infection and dangerous blood clots forming in your legs.
If you have a catheter tube draining the bladder then this will be removed as soon as possible after the operation. The catheter is removed to reduce the risk of a urine infection.
You will be seen most days by a member of the surgical team, who will monitor your operation wound and general health.
Please ask a member of staff if you are uncertain about what has happened to you, what is planned for your recovery or, indeed, if you have any questions about your care.
Rehabilitation after surgery
A broken hip is a serious injury and you will have undergone a major operation to fix it.
Although some people may return to a normal life afterwards, many find things more difficult. Recovery from your broken hip is likely to take several months. The muscles, bones and ligaments need time to heal after surgery, and you will need to build up your strength to be able to walk. Rehabilitation is hard work. You are the key to success. The rehabilitation team are there to help you recover and regain independence.
How will I get back on my feet?
Unless your surgeon advises otherwise, the physiotherapists will help you get up and out of bed the day after your surgery. They will support you to begin with until you feel more confident to use a walking frame by yourself.
You will be encouraged to practise walking up and down the ward, before being shown how to cope with stairs. Recovery can take several days or weeks, but the key is to be patient and practise the exercises that the physiotherapists show you.
The physiotherapists, nursing staff and occupational therapists will give you help and advice for a range of everyday activities that will get you back to your normal life, from dressing and washing, to cooking and shopping.
If you had dissolvable stitches, these will not need to be removed. If you had metal clips, these will be removed 10 to 12 days after the operation. You will be able to get the scar wet after this time, providing the wound is closed and dry, but you should only have a shower after advice from your nurse.
How long will I be in hospital?
Early on in your admission the team will begin to plan your discharge. The discharge co-ordinator will discuss provisional arrangements and options with you and your family.
The Occupational Therapist (OT) will come and talk to you about your home situation, and about how you feel your current injury will affect your ability to manage at home.
This will include an assessment of whether you are able to do things for yourself, such as getting washed and dressed, and getting on or off the bed and toilet independently.
If necessary you will be referred for further in-patient rehabilitation, or to community teams who can support you within your own home. The OT will advise you if there is any equipment or aids that will assist your rehabilitation, and will provide these for discharge where possible.
There is a kitchen where you are able to practise functional tasks such as making a hot drink, or simply mobilising around a kitchen environment to build your confidence for returning home and managing independently.
The therapist will discuss any concerns you have around managing shopping, cleaning and other domestic tasks, and can provide information on support services if required. You will not be sent home until we are confident that you have enough support to enable you to manage at home safely.
At our hospital, patients usually stay for 1 to 2 weeks after a hip operation. You may be able to return home sooner than this, provided you are able to walk several steps safely by yourself or with a frame, can use a toilet / commode and are able to get to bed by yourself. The community rehabilitation team will then help you with your recovery at home.
Some patients require longer stays in hospital. If you are medically unwell, you will stay in Princess Royal Hospital until you are better. If you require further rehabilitation, we may suggest that you are transferred to a rehabilitation unit near your home.
What happens when I leave hospital?
Your next of kin will be telephoned when you are due to leave hospital. You will be discharged with a two week supply of your usual tablets and painkillers. You will need to get more of these from your family doctor if you are discharged home. Some people are collected by their next of kin and others have hospital transport arranged. There is no routine follow up at the hospital after hip fracture surgery, but in some circumstances you may need to attend an outpatient appointment. We will arrange this for you, as necessary.
Will I recover completely once my broken hip has been repaired?
A broken hip is a serious injury and life changing event. You will have undergone a major operation to fix your hip. Most people find that their walking is not as good as it was before they broke their hip. Many patients need extra walking aids and extra help at home. Twelve months after hip fracture about 60% of patients still are limited in at least one type of activity (e.g. feeding, dressing, toileting). 80% of people are unable to do more complex activities such
as gardening or shopping.
How can I reduce my risk of an injury in the future?
There are several things you can do to prevent further problems after a hip fracture.
Hip dislocation
After hip hemiarthroplasty (half joint replacement), the ball of your hip joint is at risk of popping out of its socket, which would mean a return to hospital. You can reduce the likelihood of this happening by:
- Not crossing your legs. If possible, try to sleep on your back or with a pillow between your knees.
- Not bending more than a right angle at the hips, for example, to pick something off the floor. Your home may need some alterations to help you with this, which your occupational therapist will tell you about.
- Not twisting at the waist. Turn your whole body at the same time if you want to turn round.
Future fall prevention
Although most falls occur after a simple trip, some may be due to an underlying problem with, for example, blood pressure, heart rhythm, sight problems or balance problems. These may be treatable, making you less likely to fall over in future. After a short assessment while you are in hospital, we may suggest that you are referred to a ‘Falls clinic’ for further review. The arrangements will be made for you.
Thinning of the bones: Osteoporosis treatment
If you have broken your hip after a simple fall, it is likely that your bones are thinning. This is known as ‘osteoporosis’. There are several types of drugs available that can stop your bones thinning more and sometimes actually strengthen the bone, making another break less likely in future. If necessary you will be started on these tablets during your hospital stay. It is important that you get more tablets from your family doctor. People with osteoporosis usually remain on bone strengthening tablets and calcium tablets for many years.
Any questions?
If you or your relatives would like to ask any questions whilst in hospital, please don’t hesitate to ask a member of the nursing staff or your doctor.
Useful contact numbers
Royal Sussex County Hospital, Brighton, Switchboard 01273 696955
Ward L8A East Extensions 64345 or 64346
Princess Royal Hospital, Hayward Heath, Switchboard 01444 441881
Twineham Ward Extension 68248
Physiotherapy Extension 65689
Occupational Therapy Extension 68250
National Osteoporosis Society 01761 471771
Prepared by Dr Charlotte Willis, Consultant in Elderly Care. Dr Stuart White, Consultant Anaesthetist. Mr Philip Stott, Consultant Orthopaedic Surgeon. Jennifer Douthwaite, Sister Orthogeriatric Unit.
This leaflet is intended for patients receiving care in Brighton and Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.