Download and print as a PDF (383kB pdf)
On this page
- Introduction
- What is Prostate Artery Embolisation (PAE)?
- Why PAE for me?
- What are the benefits?
- Who will be doing the procedure?
- What happens before the procedure?
- What will happen on the day of the procedure?
- During the procedure
- How long will it take?
- What to expect after the procedure?
- What are the risks of PAE?
- Uncommon risks:
- Who should I contact for further information or advice?
Introduction
This leaflet is about Prostate Artery Embolisation, it explains what the procedure consists of, the benefits and the risks. This leaflet should be used as the starting point of an informed discussion between you and your doctor: direct any queries you have to the doctor or department that has referred you.
As you read this leaflet, it may be useful to consider these questions:
• What are my options?
• What are the possible benefits and risks of those options?
• What help do I need to make the decision?
What is Prostate Artery Embolisation (PAE)?
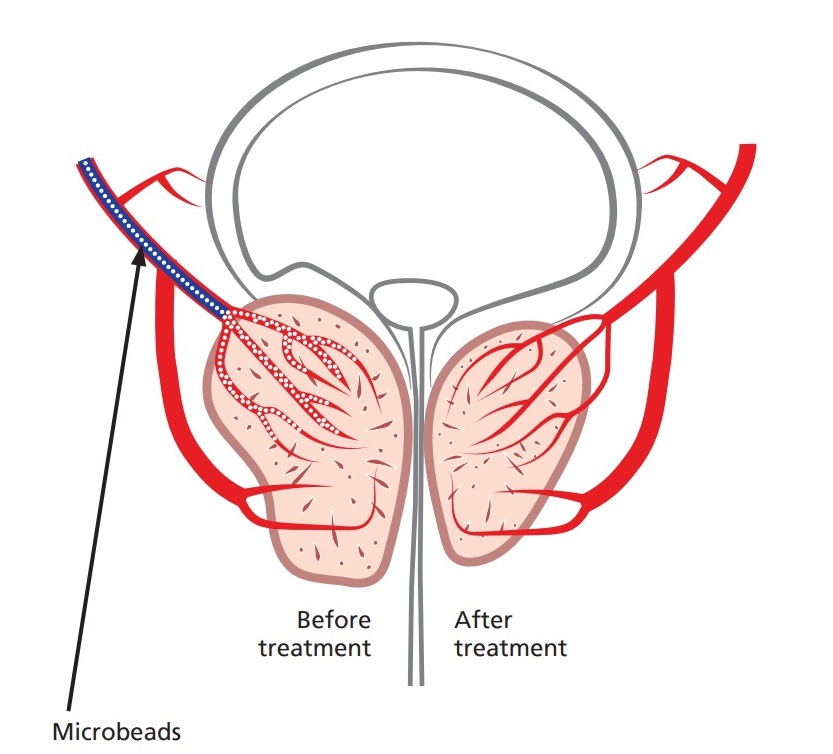
PAE is a non surgical technique to treat an enlarged and troublesome prostate by blocking off the arteries that supply the gland: this makes it shrink.
PAE is a less invasive procedure than other treatments for an enlarged prostate (e.g. TURP). PAE can be carried out as a day case and carries a lower risk of certain complications (e.g. retrograde ejaculation, incontinence and impotence).
Why PAE for me?
Tests that you have taken, have shown that you have an enlarged prostate. Your symptoms may include passing urine very frequently (especially at night), passing only small volumes of urine and having a poor flow / stream of urine.
PAE is a good option for those with a very big prostate gland, where treatment with medication or prostate operations (e.g. laser surgery) may not be successful or could have
increased risks.
What are the benefits?
After PAE, the prostate gland should begin to shrink over the next few weeks. Studies show that more than 70% of men will see improvement in their symptoms after PAE.
Recent research has demonstrated that the majority of patient requiring a long term catheter can have this removed within a few weeks.
Who will be doing the procedure?
PAE will be carried out by an Interventional Radiologist, a specially trained doctor with expertise in the use and interpretation of X-ray imaging to guide the embolisation operation.
What happens before the procedure?
You will require a particular CT scan (CT Angiogram) to visualise the arteries in your pelvis. This will inform the radiologist whether this treatment is suitable for you.
The Interventional Radiologist will discuss the procedure in person when you attend for the planning CT scan or by telephone.
You will require a blood test prior to the procedure to check your kidney function and that you are not at increased risk of bleeding. This additional check may take place with your GP surgery.
A telephone pre-assessment will take place with one of our interventional radiology nursing team to review your medications and medical history. This is also an opportunity to clarify any post procedure care and transport requirements.
You will be asked to complete a questionnaire on your symptoms. This will help to inform us on the success of the procedure.
What will happen on the day of the procedure?
You should not eat anything 4h prior to the procedure.
You may continue to drink water, take your normal medication unless we tell you not to.
You will arrive at the Imaging Department and will be accompanied to our day case area.
Inform us of any allergies.
A Radiologist will explain the procedure and associated risks again, and you will be able to ask questions. If you choose to have the procedure you will need to sign a consent form.
You will be asked to change into a hospital gown and a small tube (cannula) may be placed into a vein in your arm to administer medications, sedatives to relieve anxiety, painkillers if required
Once all checks have been completed, you will taken to the angiography suite for the procedure. There will be nurses, a radiographer and at least one interventional radiologist with you throughout the procedure; a trainee doctor may be present.
During the procedure
• You will need to lie on your back on an X-ray table for the duration of the procedure which usually lasts 2 to 3 hours.
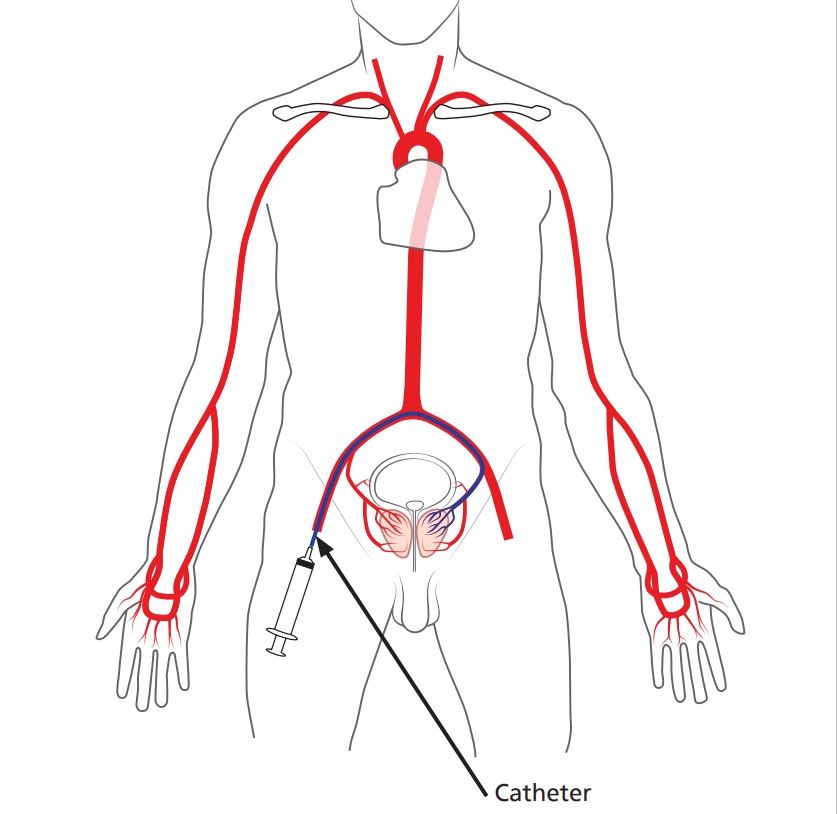
• The skin around your groin or wrist will be cleaned with antiseptic solution and covered with sterile drapes.
• Using an ultrasound machine, the radiologist will inject a local anaesthetic into the skin and deeper tissue over the artery: this will sting and the area will then go numb.
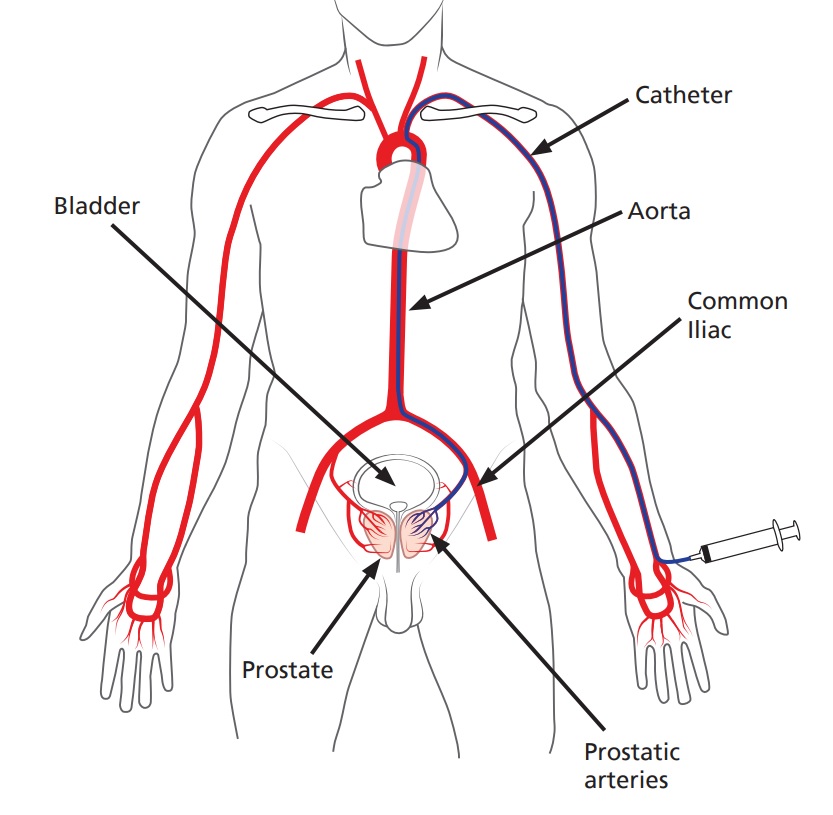
• A small tube (catheter) is inserted into the artery and navigated through your blood vessels with the aid of an X-ray machine to locate the arteries that supply blood to the prostate gland.
• X-ray dye will be injected into your arteries during the procedure to aid navigation of the catheter. At times you may be asked to hold your breath and you will need to keep still to assist the Radiologist’s view. It is common for the dye to cause a temporary hot sensation.
• Usually, both left and right prostate arteries can be reached from one artery in the groin, but sometimes we need to access the artery in your other groin too.
• Once the prostate blood supply has been confirmed, fluid containing thousands of tiny particles is injected through the catheter into the arteries that supply the prostate. This blocks these blood vessels and the prostate is starved of its blood supply.
• When the injection to both the left and right arteries is complete, the catheter is removed from the artery. A special arterial stitch / plug (closure device) is commonly used to stop
bleeding from the artery, or pressure by hand will be applied.
• Infrequently a urinary catheter may need to be inserted for this procedure and will be removed before you are discharged.
How long will it take?
Every patient is different, and it is not always easy to predict; expect to be in the Radiology Department for 2 to 3 hours.
What to expect after the procedure?
You will be taken to Main Theatres Recovery so that nursing staff can monitor you closely.
• If you are in pain, you will be given appropriate painkillers.
• You will be required to stay in recovery for 4 hours, occasionally a one night stay in the hospital may be necessary.
• There may be a small bruise in the groin around the access site: this is quite normal.
• You will have antibiotics prescribed, these are to be taken for 5 to 7 days following the procedure.
• You will be able to resume most normal daily activities within 24 to 48 hours. We recommend avoiding driving and all strenuous activities for 48 hours.
• We advise you take one week off work following the procedure.
• You will be telephoned 1 week after the procedure by a nurse to check on your recovery. You will then have an ultrasound of the prostate gland around 3 months after the procedure where you will repeat the questionnaires. The Interventional Radiologist will contact you by telephone at 3 to 6 months to discuss your symptoms and response to the treatment.
What are the risks of PAE?
PAE is a relatively new procedure for prostate enlargement. Current evidence, reviewed by the National Institute for Health and Care Excellence (NICE), clearly shows that PAE is safe and an effective treatment option. As with any other medical procedure complications may arise.
You may experience some discomfort in the lower abdomen or when urinating: this normally resolves after 10 days. Regular paracetamol can help with the discomfort.
Uncommon risks:
There is a low risk of developing retrograde ejaculation (less than 15% in UK centres). This is much lower than the risk with TURP (up to 48%).
• In 1% of cases, patients can develop urinary incontinence.
• In up to 10% of cases, the arteries that supply the prostate are too small or diseased to access the prostate meaning we are unable to treat the arteries. If this is the case, the Urologist may discuss the option of TURP instead.
• The prostate can become swollen immediately after the procedure, making passing urine difficult: a urinary catheter may be necessary until the swelling settles down. If you are having trouble passing urine after discharge from hospital you will need to attend A and E.
• There is the possibility of having blood in the urine after PAE, this usually settles by itself.
• Blocking arterial flow to the prostate makes the gland more prone to infection: antibiotics will be prescribed for you to take after the procedure.
• There is a less than 1% risk of blocking blood vessels and blood supply to other organs inside your pelvis (including urinary bladder, bowels or genitals). This is a serious complication and so a CT scan of your blood vessels will be performed before and during the procedure to reduce this risk.
• Post embolisation syndrome is seen in up to 25% of cases: patients report flu like symptoms for up to a week following PAE.
Who should I contact for further information or advice?
Out of hours, please attend your nearest Accident and Emergency department.
Further on-line resources
References
NICE (2018) “Interventional procedure overview of prostate artery embolisation for lower urinary tract symptoms caused by benign prostatic hyperplasia”
Ray et al (2018) “Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE Study)” BJU Int 2018; 122: 270-282
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.