Download and print as a PDF (451kB pdf)
On this page
- What is malrotation?
- What causes malrotation?
- What are the symptoms of malrotation?
- How is malrotation and volvulus diagnosed?
- How is malrotation treated?
- What happens before surgery?
- What happens during the operation?
- Are there any risks?
- What happens afterwards?
- How long will my baby be in hospital?
- What about follow up?
What is malrotation?
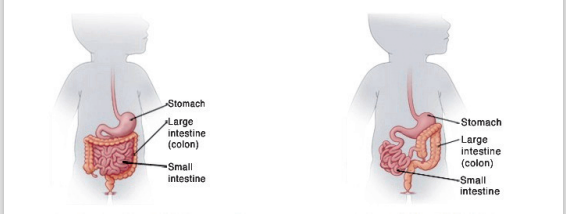
Malrotation is an abnormality of the bowel which happens while the baby is developing in the womb. Early in pregnancy the bowel is a long straight tube leading from the stomach to the rectum (bottom). The bowel then moves into the umbilical cord temporarily while it develops into the large and small bowel.
Around the tenth week of pregnancy the bowel moves back into the abdomen and coils up to fit into the limited space there. If the bowel does not coil up in the correct position this is called malrotation. Volvulus is a complication of malrotation and occurs when the bowel twists so the blood supply to that bit of the bowel is cut off.
What causes malrotation?
We do not know exactly what causes malrotation and volvulus but it is not due to anything that happened during pregnancy. It affects about one in 2,500 to 3,000 babies, boys and girls in equal numbers.
What are the symptoms of malrotation?
Malrotation may not have any symptoms. Many people are never diagnosed with malrotation because it causes no problems.
However because of the small bowel’s abnormal position it may kink or twist causing a blockage. This means that feed cannot easily pass through the duodenum to the rest of the bowel. Your baby may have episodes of crying and drawing their legs up to their body which then stop suddenly. Your baby may vomit green fluid and pass little or no stool (poo) as it cannot pass the twisted area. Your baby may also show signs of dehydration with less frequent wet nappies and the soft spot (fontanel) on the top of the head maybe sunken. Your baby may also become quiet and sleepy.
How is malrotation and volvulus diagnosed?
Malrotation and volvulus are usually diagnosed following x-rays. A contrast study of the bowel may also be helpful as it shows where the feed is unable to pass. An ultrasound scan may also be done to help with diagnosis.
How is malrotation treated?
If there is a malrotation without volvulus the surgeons will discuss treatment options with you and the neonatologists. It may be necessary to have an operation to correct the malrotation or have a period of ‘watching’. If volvulus is involved then surgery is needed. The tissue of the bowel can die from lack of blood supply leading to it not functioning correctly and possibly infection. This has to be corrected surgically and is a life threatening condition.
What happens before surgery?
Your baby will have already been started on intravenous (drip in the vein) fluids and be nil by mouth (without feeds). They will have had a nasogastric (NG) tube passed through a nostril down into their stomach to relieve any pressure and remove any bile (thick green fluid) that maybe building up in the stomach.
The surgeon will explain the procedure and what they expect to find. They will ask you to read and sign a consent form. The operation is performed here at the Royal Alexandra Children’s Hospital.
The operation will be done under general anaesthetic. During surgery your baby will be cared for by an anaesthetist, who will place him/her on a ventilator (breathing machine) to allow the surgeon to operate. Your baby will have a general anaesthetic and be asleep throughout the operation; he/she will feel no pain or discomfort.
What happens during the operation?
The operation is called a Ladd’s Procedure. The surgeon will straighten out the twisted bowel and check for any unhealthy areas. If the bowel looks healthy it will be put back into the abdomen in a safe position. An appendectomy (appendix removed) is also usually done as the appendix is often on the wrong side of the body in malrotation. This could cause problems in diagnosing appendicitis (infection of the appendix) later in life.
If areas of the bowel tissue have died the surgeon will remove these. They will try to leave as much of the bowel as possible.
Are there any risks?
These will be discussed with you by the surgeons when they take consent and by the anaesthetist. Risks may include:
• Bleeding or Infection during or after the operation.
• Adhesions, where bands of tissue may block the bowel, may develop. If these do occur a further operation would be needed to correct the problem.
What happens afterwards?
Your baby will be transferred back to the intensive care nursery to be looked after and he/she will be ventilated (on a breathing machine) as long as necessary. The NG tube will continue to drain any bile from the stomach on a regular basis. This is perfectly normal at this stage and the amount will get less and less as baby gets better.
Once the surgeons are satisfied that the bile drainage is small and they can hear bowel sounds, they will allow small amounts of milk to stimulate the bowel to work. This amount will be increased slowly as tolerated. This can sometimes take several weeks. If your baby has lost any or a significant length of bowel this process will take longer.
How long will my baby be in hospital?
This varies depending on your baby’s operation and the amount of time the bowel needs to manage (tolerate) milk. In uncomplicated cases it usually takes four to six weeks. If the process takes very long, then he/she may be transferred to the children’s hospital for the remainder of their care before discharge home.
What about follow up?
Your baby will be followed up in the outpatient clinic by the Neonatal and Surgical teams at 6 to 8 weeks after discharge and you will of course be seen by your health visitor at home. The nurse and neonatal team looking after your baby will be happy to answer any further questions you may have.
Trevor Mann Baby Unit
01273 696955
Ext. 64377
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.