Download and print as a PDF (267kB pdf)
On this page
- What is Gastroschisis?
- How is this condition diagnosed?
- What happens during pregnancy?
- What are the major problems with gastroschisis?
- How will my baby be born?
- What happens at the birth?
- Will my baby need an operation?
- What happens during treatment?
- Will my baby be in pain?
- When will my baby start milk feeds?
- How long are we expected to stay in hospital?
- Which other professionals may be involved in my babyâs care?
- What is the final outcome?
- What about follow up?
- Where can I get additional support?
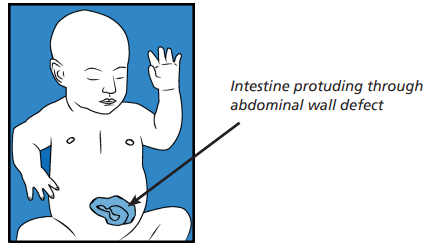
What is Gastroschisis?
Gastroschisis is a condition where your baby develops a defect (hole) in the abdominal wall during development, while still inside your womb. This is usually to the right side of the umbilical cord and some of the bowel escapes through this hole and continues to develop outside your baby’s abdomen.
This happens in approximately 1:7000 births. There is an increased chance that your baby will be born premature and low in weight.
How is this condition diagnosed?
Gastroschisis is usually diagnosed during pregnancy at your routine 16 to 20 week scan. Once diagnosed you may be offered a more detailed scan and your obstetrician will discuss with you if any other tests are needed.
What happens during pregnancy?
The escaped bowel floats in the amniotic fluid in your womb for most of the pregnancy. Sometimes the fluid irritates the bowel and makes it inflamed and thick. Sometimes the bowel becomes twisted as it floats and the blood supply may be restricted. You will have several ultrasound scans during your pregnancy to monitor baby’s growth and the amount and condition of the bowel lying outside in the amniotic fluid. Monitoring will help determine the best time and place for your baby’s deliver
What are the major problems with gastroschisis?
There are two important issues after birth:
- Returning the bowel back into the abdomen and repairing the defect. This is either by a primary or staged procedure (these terms will be explained later.)
- Establishing your baby onto milk feeds. This can often take a long time (several weeks to months) as the bowel which was outside the abdomen may not work properly. By a drip your baby will be given nutrition.
This is called TPN (total parentral nutrition), it contains all the nutrients your baby needs to grow. It is given through a special intravenous feeding line called a long line. Prolonged TPN can have its own problems such as infection, blockage of lines and liver failure.
How will my baby be born?
A normal vaginal delivery is possible and the options will be discussed with you. The decision will be based on what is best for the baby and mother.
What happens at the birth?
Following delivery the neonatal team caring for your baby will ensure that your baby is breathing normally. Babies need variable amounts of support with their breathing depending on how prematurely he / she is born.
An NG tube (nasogastric tube) will be passed up your baby’s nose and down into their stomach. The NG tube will be secured in place and is used to get rid of excess air which could make your baby’s bowel more swollen. The baby’s abdomen and exposed bowel will be wrapped in a medical clingfilm to prevent further damage and infection. This also helps to keep your baby warm.
If your baby is well enough he / she may be handed to you for a cuddle. If it is not possible to have a cuddle the neonatal team will show your baby to you on the way up to the neonatal unit.
Will my baby need an operation?
The surgeon and surgical team will assess your baby’s condition and will decide on one of two types of operation, Primary Repair or Staged Repair. There is no alternative treatment for this condition. They will discuss the operation with you and they will ask you to read and sign a consent form.
The operation is performed at the children’s hospital but in some cases, where straight closure is not possible, a procedure may be carried out on the neonatal unit.
During surgery your baby will be cared for by an anaesthetist, who will place him / her on a ventilator (breathing machine) to allow the surgeon to operate. Your baby will have a general anaesthetic and be asleep throughout the operation, he / she will feel no pain or discomfort.
If there is only a small amount of bowel outside the abdomen, this will be put back and the abdomen and the wound closed. The sutures (stitches) used do not have to be taken out as they are dissolvable. A dressing maybe placed over the wound. This is called a Primary Repair.
What happens during treatment?
An intravenous feeding line (long line) will be inserted so your baby can have TPN and medications while the bowel returns to full fuction. This will remain in place until he / she is able to manage (tolerate) full milk feeds.
Sometimes if the gastroschisis is large, or the abdominal cavity is small the surgeons will place a pouch around the bowel. The pouch is then suspended from the ceiling of the incubator and gravity along with a phased reduction in the size of the pouch will help the bowels to slip back inside the abdomen. This may take a few days in total and only then will the final closure occur.
Occasionally there is not enough skin to cover the affected area and a patch of silicone meshing or a gortex patch is stitched to the skin. Over the next few months the skin will slowly grow over the patch. This is called a Staged Repair.
In addition, if the blood supply to the bowel has been impaired and part of the bowel has died or is completely blocked that segment of bowel will be removed at surgery.
Your baby will be cared for in the intensive care nursery where their breathing will be supported, initially by a ventilator. He / she will be closely monitored and fed intravenously through the broviac line. Regular blood tests will also be carried out.
Will my baby be in pain?
Your baby should not be in pain after the operation. He / she may remain ventilated for a few days to allow him / her to recover safely. The doctors and nurses will give pain relieving medicines for as long as it is needed. This will probably start as a morphine infusion and then be reduced to less strong pain killers over time.
When will my baby start milk feeds?
As the bowel was outside the abdomen for a long time it does not work properly initially and may take anything from one to three weeks or sometimes longer to begin working again.
The NG tube allows thick green fluid, called bile, to be drained from the stomach on a regular basis. This is perfectly normal at this stage and the amount will get less and less as baby gets better.
Once the surgeons are satisfied that the bile drainage is small and they can hear bowel sounds, they will allow small amounts of breast milk to stimulate the bowel to work. This amount will be increased slowly as tolerated. This can sometimes take several weeks. If your baby has lost a significant length of bowel this process will take longer.
Although breast feeding is normally encouraged, some babies cannot absorb breast milk very easily and to start with they may need to have a special formula. If you wish to breast feed; the midwives and nurses will help you to establish expressing your milk via a pump. This will be frozen until your baby is allowed to start some milk.
The nurses will help you care for your baby with nappy changing and gentle washing. As your baby’s condition improves and you become more confident the nurses will help you less and less.
How long are we expected to stay in hospital?
This varies depending on how premature your baby is and the amount of time the bowel needs to manage (tolerate) milk. In uncomplicated cases it usually takes six to eight weeks but may take several months particularly if a lot of bowel had to be removed. If the process takes very long, then he / she may be transferred to the children’s hospital for the remainder of their care before discharge home.
Which other professionals may be involved in my baby’s care?
Besides the surgeon and neonatologist your baby will be looked after by neonatal nurses. Additional help and advice may be sought from a dietitian and gastroenterologist.
What is the final outcome?
Improvements in obstetric and neonatal care have increased the early survival of babies. The administration of TPN allows babies to survive and grow even when the bowels cannot be used for several weeks. Once the wound has healed and the baby is able to manage milk feeds they make good progress and are expected to live a normal lifestyle.
Those with more severe problems will be dependant on partial or total TPN support for several months and even years, with it’s attendant problems of infection, broviac line blockage and liver problems.
In some cases of gastroschisis, there is not sufficient bowel to sustain normal life. Bowel transplant is approaching being a viable medical treatment. However, this treatment is not without significant problems and finding a suitable donor is difficult.
What about follow up?
Your baby will be followed up in the outpatient clinic to monitor his / her growth and development.
You may be referred to the children’s community nurses if this is appropriate for you and you will of course be seen by your health visitor at home.
Where can I get additional support?
You can talk to your baby’s doctors and nurses for additional information. An interpreter can be arranged as necessary. The unit has a counsellor who can provide support if requested.
There is a parent support group for this condition called ‘GEEPS’ (Gastroschisis Exomphalos Extrophies Parents Support). Information is available on their Facebook page
The nurse and neonatal team looking after your baby will be happy to answer any further questions you may have.
Trevor Mann Baby Unit
Telephone:
01273 696955
Ext. 4377
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.