Download and print as a PDF (526kB pdf)
On this page
- What is this information about?
- Who should I contact if I have any further questions after I've read this information?
- What is chronic hepatitis B virus (HBV)?
- How did I get HBV?
- What can I do to stop me giving HBV to others?
- What symptoms might I experience?
- How is HBV diagnosed?
- How is HBV managed?
- How is the medication supplied?
- What can I do to support a healthy liver?
- What if I am pregnant, thinking about getting pregnant or breastfeeding?
- Frequently asked questions:
- Where can I find further information and support?
What is this information about?
This information is about Chronic Hepatitis B Virus (HBV), including how you may have been infected, symptoms, diagnosis, and management options. It has been developed by the hepatitis team, which includes doctors, nurses and pharmacists.
Who should I contact if I have any further questions after I’ve read this information?
If you have any further questions, please do not hesitate to contact us for further advice and / or resources. Contact details are below.
What is chronic hepatitis B virus (HBV)?
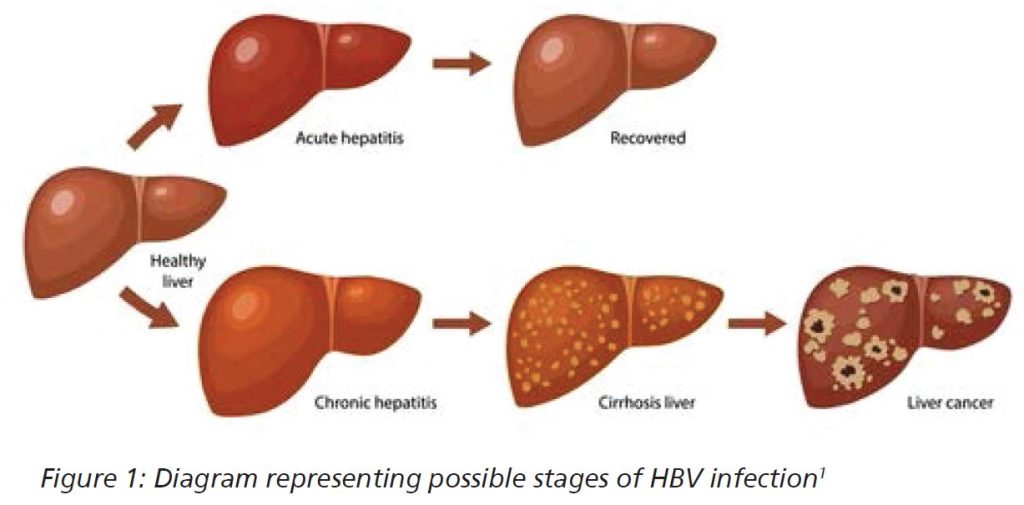
HBV is a virus found in the blood and other bodily fluids. It can cause inflammation of the liver which may lead to liver stiffening (fibrosis) and possibly other risks such as cirrhosis and cancer.
Some people infected with HBV will clear the virus naturally themselves. However, if infection continues for more than 6 months they are considered to have a chronic infection even if they do not show any symptoms.
The World Health Organisation (WHO) estimates that approximately 240 million people across the world are chronically infected with HBV and so it is an important global health problem.
How did I get HBV?
As HBV is a blood-borne virus associated with infected blood and some bodily fluids, the common causes of transmission from a HBV carrier are listed below:
- Childbirth (from mother to new-born baby).
- Unprotected sex (without a condom).
- Sharing needles (via injecting drugs, tattoos, piercings).
- Sharing toothbrushes or razors.
- Receiving infected blood or blood products (before the introduction of screening).
You also may be at higher risk of getting HBV if you live or have lived in areas of the world where HBV is common.
What can I do to stop me giving HBV to others?
Things you can do to protect others:
- Avoid having unprotected sex unless you are sure your partner has been vaccinated against HBV.
- Avoid re-using or sharing drug-taking equipment. If you find yourself in a situation where you have to re-use any equipment, make sure you only use your own and no one else’s.
- Avoid sharing razors and toothbrushes with other people.
- Advise sexual partners and household members to be vaccinated for hepatitis B through their GP.
- Clean and cover cuts and other wounds. If your blood is spilt, clean it up yourself with household bleach immediately.
- Let healthcare professionals know you have HBV.
What symptoms might I experience?
Many people who are infected with HBV do not show any symptoms. However, if you are to develop symptoms it is usually within the first 5 months2 after exposure and could include:
- Flu-like symptoms (tiredness, fever, general aches and pains).
- Loss of appetite.
- Feeling or being sick.
- Diarrhoea.
- Abdomen pain.
- Dark urine.
- Clay-coloured bowel movements.
- Yellowing of the skin or eyes (jaundice).
Be Advised
Even if you are not showing symptoms, this does not mean the HBV isn’t causing damage to your liver.
How is HBV diagnosed?
Hepatitis B virus is diagnosed by detection of hepatitis B surface antigen (HBsAg) in your blood. This test can be taken at your GP surgery, hospital, outreach clinic or sexual health clinic.
If you have a positive HBsAg test, then you will be referred to the specialist team and a full blood-borne virus screen will be completed, including hepatitis A, C, and D, HIV and liver function tests (LFTs).
To understand the stage of your HBV and possible liver damage, you will likely undergo the following:
- Fibroscan (a scan to check the stiffness of your liver).
- Ultrasound scan (a scan to check for any abnormalities in your liver).
- Liver biopsy may sometimes be required.
How is HBV managed?
Currently there is no cure for HBV but research is continuing. Medication is available to suppress the virus and stop ongoing damage to the liver and many patients are therefore on long-term treatment. Not everyone needs medication however, and this will depend on your test results and medical history.
If treatment is advised, you will be involved in the decision process. The specialist team will review your bloods to determine the most appropriate treatment and dose.
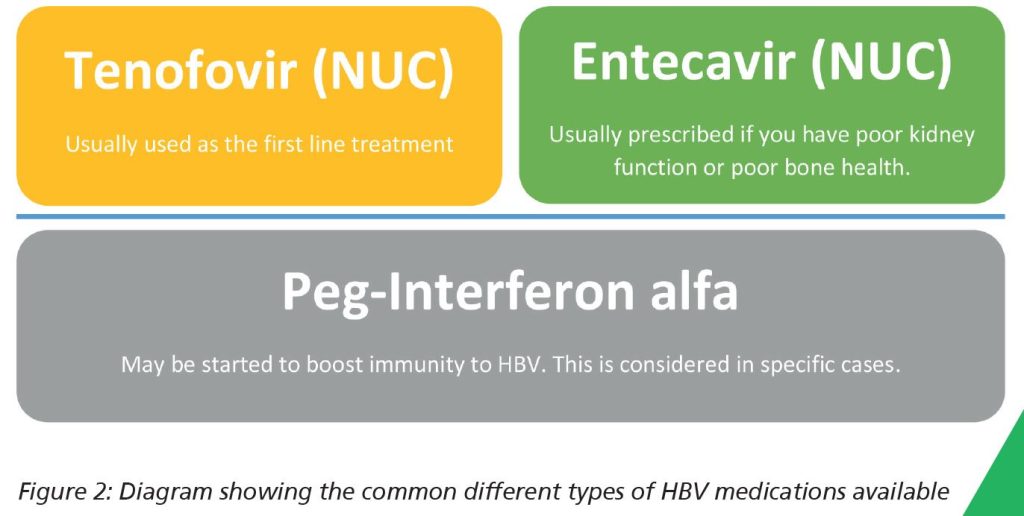
The main group of medications are called Nucleoside analogues (NUC) and work by reducing the replication of hepatitis B virus in your body. Some patients may require an additional medication, peg-interferon alfa.
There is separate information available for individual medications. Please request this from your specialist team.
How is the medication supplied?
It will be supplied via your hospital specialist team only. It is not supplied by your GP.
You will need to have regular blood tests before medication is supplied so please keep up-to-date with these tests which are done at least every 6 months, sometimes more regularly. Your specialist team will let you know when they are required.
Be advised
Please contact the delivery team if you are due to run out in 2 weeks and have not heard about delivery. Contact details are at the end of this information.
What can I do to support a healthy liver?
There are several things you can do to support a healthy liver, these include:
- Eat a healthy, balanced diet.
- Avoid drinking alcohol.
- Stop smoking.
- Exercise regularly.
- Maintain a healthy weight.
- Attend your follow-up appointments and complete your required tests.
What if I am pregnant, thinking about getting pregnant or breastfeeding?
People with HBV can usually have a healthy pregnancy and breastfeed, however it is advised to discuss plans with your specialist team first as they will need to monitor your HBV closely and if you are taking medication, this may need to be changed. Babies born to HBV positive people will need to be vaccinated within 12 hours of birth. The hepatitis B vaccine is given to infants in the UK as part of their routine childhood vaccination schedule.
Frequently asked questions:
Why is it important to attend appointments?
Whether you are on treatment for HBV or not, it is important for you to attend all scheduled appointments.
This enables your specialist team to monitor your liver with blood tests and surveillance scans, and to continue the discussion around your liver health, including whether treatment should be started. If you are on treatment then further supplies of your medication can be arranged at these appointments, as your GP is not able to prescribe these specialist medications.
Who is included in the specialist healthcare team?
- Hepatologists (specialist liver doctors).
- Nurses.
- Pharmacists.
- Administration team.
- Research team.
All members of the team will feedback to each other to ensure appropriate monitoring and management of your condition and link with your GP.
Where do I get my medications from?
Be advised
Your medications will be supplied via your hospital specialist team only. They are not supplied by your GP.
Please contact the delivery team if you are due to run out in 2 weeks and have not heard about delivery. Contact details are at the end of this information.
What monitoring is needed?
Regular blood tests are done at least every 6 months, and you may also need regular scans to check your liver health, including fibroscans and ultrasound scans. Your specialist team will develop a personalised care plan for you and let you know the frequency and type of monitoring required.
If you are taking HBV treatment, you will need to get regular blood tests before medication supply so it is important to keep up-to-date with these tests.
What if I plan on moving home?
- Same city: please let us know the new address so we can send medication, test forms and letters to the correct address.
- Different city: please let us know as soon as possible as we will need to transfer your care to the local service in your new area of residence.
What if I plan on leaving the country for more than 3 months?
Please discuss this with your specialist team as soon as possible.
Is there any research looking at a cure for HBV?
There are currently trials underway looking at potential options to cure hepatitis B completely. However, many of these are still in the early stages and therefore it is likely to be many years before we can offer these treatments.
Where can I find further information and support?
Please refer to patient information leaflet found inside medication box.
More information can be found via:
The Specialist Team
Answerphone service: please leave a message and someone from the team will respond during normal working hours Monday to Friday 09:00 to 17:00
Answerphone
01273 664541
- Out of hours GP (if open)
- NHS 111
- The medication delivery team: space to write in their name
More information about HBV can be found via The British Liver Trust website .
A patient information leaflet on HBV is available. Please request these from the specialist team or find it here .
Be aware
Keep all medicines out of the reach of children.
Never give any medication prescribed for you to anyone else. It may harm them even if their symptoms are the same as yours.
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.