Download and print as a PDF (407kB pdf)
On this page
- What is a chest drain?
- What is my injury?
- Will these injuries require a chest drain?
- What happens during the procedure?
- Will it hurt?
- Are there any risks during the procedure?
- How will the drain be attached?
- How long will the drain stay in?
- Who will look after my chest drain?
- Important things to know about your chest drain
- How will the drain be removed?
- Deep breathing exercises (DBEs)
- What happens when I go home?
What is a chest drain?
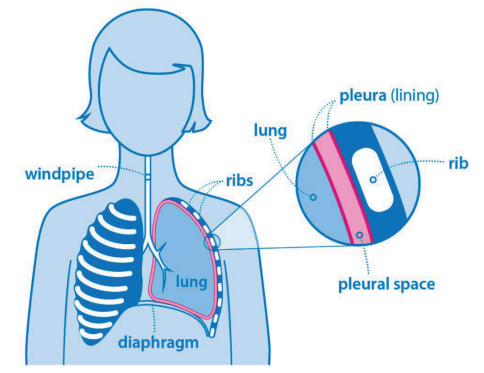
An injury to the chest can cause blood or air to gather inside the area around the lungs, called the pleural space. To remove this, we may need to insert a chest drain. This means placing a tube (called a drain) through the skin and lung lining (called the pleura) into the space between your lungs and rib cage.
There are many structures inside the chest that can be injured including the heart, lungs and ribs.
What is my injury?
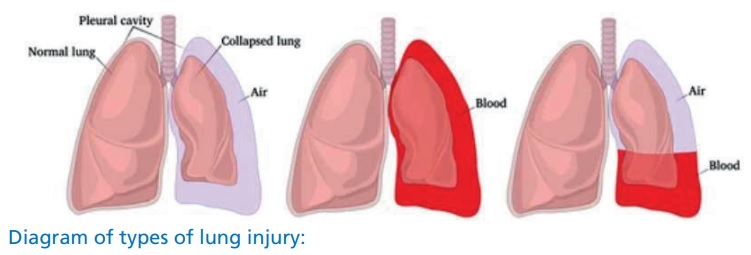
There are three main types of lung injury:
Pneumothorax: often called a collapsed lung, a pneumothorax means that air is collecting inside the chest, around the lung, instead of being breathed out through the mouth and nose.
Haemothorax: this is where blood from a damaged vessel collects inside the chest, around the lung.
Contusions: bruises to structures like the lungs or heart. Contusions do not usually require treatment but can be painful and may require monitoring.
Chest and lung injuries usually mean that you feel pain and have difficulty in breathing. You may require oxygen.
All these injuries can occur without or without rib fractures (broken ribs). Rib fractures can also occur on their own, without other associated injuries. Rib fractures rarely require surgical treatment but are very painful.
Sometimes with chest injuries, air can escape from the chest and under the skin of the chest, neck and face. This is called surgical emphysema. This requires close observation but is not usually life threatening, and the body will reabsorb the air into the bloodstream.
Will these injuries require a chest drain?
Pneumothorax, Haemothorax or Haemopneumothorax (which is a combination of air and blood) will often require a chest drain. Chest drains are usually inserted when you arrive at the Emergency Department, but can be inserted later in your hospital admission if the injury doesn’t improve or your symptoms get worse.
What happens during the procedure?
Once it has been decided that you need a chest drain, the doctor will discuss the reasons and possible complications with you before asking for your consent to begin.
If you have been severely injured or are very unwell, the chest drain may be inserted urgently without being discussed with you first. This can be discussed at any time during your recovery with your team.
The procedure will be carried out by a qualified doctor with a suitable level of experience. Because this is a Teaching Hospital, the doctor performing the procedure will be supervised by a senior doctor.
A sterile drape will be placed over your chest and may cover your face. This can feel a bit strange, but the team of doctors and nurses will be with you the whole time to provide reassurance.
Your skin will be cleaned and then a local anaesthetic will be injected to numb the area. The drain (a sterile tube) will then be inserted between the ribs in the anaesthetised area into the chest. It is then connected to a longer tube which then attaches to a drainage bottle containing sterile water. The water acts as a one-way seal to allow air or fluid to drain out but not go back
into your chest.
Will it hurt?
The local anaesthetic will sting at first and you may feel some pushing and pulling during the procedure. Please inform the doctor if you feel any pain either during the procedure or at any time after insertion. We can give you plenty of pain killers to help with any discomfort.
Are there any risks during the procedure?
There are some risks associated with chest drain insertion. However, the collection inside your chest needs to be drained, and a chest drain is the safest way to do this.
Risks such as infection, either at the insertion site or inside the chest itself, bleeding or drain blockage can sometimes occur.
Every effort is made to prevent this from happening. Rarely, air can leak from the drain into the surrounding tissues, known as surgical emphysema (detailed earlier in the leaflet). Always report any concerns to your nurse or clinical team.
How will the drain be attached?
We use a stitch to tie the drain in and an adhesive dressing on the skin to make it as secure as possible. We may also attach the tube to your side with some tape to allow some slack as you move. However, please move carefully.

How long will the drain stay in?
How long you need your chest drain depends on how your symptoms and condition improve. The average is three to seven days. Your clinical team will keep you informed on a regular basis. You will stay in hospital as long as your drain is required. You may require one or more chest x-rays to make sure the drain is working correctly.
Who will look after my chest drain?
Chest drains are managed by the Upper GI Surgical team. They will review you daily and decide what needs to happen that day.
You will be cared for by a ward nurse and a healthcare assistant. They will assist you with washing, dressing, taking medication and monitoring your pain. The nurse will also monitor your drain every four hours.
You will meet one of the Major Trauma Practitioners (MTP). The MTPs review all the Major Trauma patients in the hospital, offering advice to patients and staff. They will follow your progress throughout your hospital stay and spend time discussing your injuries with you and answering any questions you may have.
Advanced Care Practitioners (ACPs) may also assess your chest drain. ACPs work in designated wards and teams and provide clinical expertise and education.
You may also meet the Acute Pain Team to help you manage your pain. You can ask any of these team members questions at any time.
Important things to know about your chest drain
- You may see air bubbling out through the bottle although this is normal and shows that air is leaving the chest. Fluid or blood may also drain into the drainage bottle. This is normal unless a lot comes out very quickly. If this happens please inform your nurse straight away.
- If you are in pain please ask your nurse, doctor or MTP for painkillers. Some pain is to be expected with chest and lung injuries, but you should be able to take deep breaths and move without too much discomfort.
- The drain can accidentally come out if pulled or twisted so please take care. If the drain does come out or becomes disconnected tell someone straight away.
- You need to keep the drainage bottle below the level of the drain (at the point it enters the chest). Usually it is placed on the floor. Please be mindful when moving around that you need to take care not to lift the bottle too high. Please ask staff for help if you need to move or walk to the bathroom.
How will the drain be removed?
This is straightforward and is usually done by the doctor or nurse on the ward. Once all the dressings are removed the drain will be gently pulled out. You may be asked to hold your breath in a special way when this is done. It can be an uncomfortable or strange feeling but only lasts a few seconds.
A clean dressing is applied that must remain in place for at least three days. If you are being discharged we can provide you with extra dressings. Showering should be brief whilst the dressing is in place.
Deep breathing exercises (DBEs)
Deep breathing exercises are essential to try and prevent getting a chest infection. We would advise that you aim to take 5 to 10 deep breaths every hour you are awake. You should also try to cough. If coughing is too painful, a ‘huff’, as if you are cleaning a mirror, can also be effective.
Your nurse or physiotherapist may also give you a spirometry device. This is another kind of DBE. You will be instructed how to use it and given challenges to complete as you recover.
If you are in too much pain to complete your DBEs you must inform your nurse. You can have as much pain killer as you need to complete your DBEs.
What happens when I go home?
Most people do not have a repeated occurrence of the haemo/pneumothorax, but very occasionally it can happen. You will notice a change in your breathing: if this happens please call 111 or 999.
Some degree of pain is normal for a few days after leaving hospital. This can usually be managed with the painkillers we have sent you home with. If you have a lot of pain, notice any bleeding, difficulty breathing, or fever please call 111 or 999 immediately. This pain usually improves in the first week and should continue to become more manageable over the next few weeks. You should be able to wean your painkillers down over time.
You may have to modify your level of activity, take time off work and rest more than normal. But it is important to stay as active as you can to prevent issues such as blood clots or chest infections. Your clinical team and Physiotherapists can advise you if you have any questions about your mobility and exercise.
Continue your deep breathing exercises until you are back to your normal level of activity.
Contact your GP if you have any concerns after leaving hospital. You can remove the dressing yourself three days after leaving hospital.
If you are worried about taking time off work, or any financial or legal issues, please ask to speak to an advisor from the Major Trauma Signposting Partnership, a helpful team that can answer non-medical questions, or request a leaflet with their contact information.
Major Trauma Signposting Partnership (MTSP)
Phone
0330 043 2829
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.