Download and print as a PDF (365kB pdf)
On this page
What is bladder pain syndrome?
Bladder pain syndrome is a condition characterised by pain in the bladder, especially before passing urine, usually in association with frequency and/or urgency of micturition.
It is not uncommon to have other types of pain as well, such as pelvic pain and painful intercourse. The condition can cause considerable distress to patients and affect their quality of life.
What causes bladder pain syndrome?
The cause of this condition is unknown. In the past, the condition was called ‘interstitial cystitis’. This term implied that the condition was caused by an infection, which was never proven, hence the change of name to ‘bladder pain syndrome’.
Attention is now focused on the protective layer that lines the inside of the bladder. It is believed that low levels of this layer makes the bladder very sensitive and easily irritated.
How is the diagnosis made?
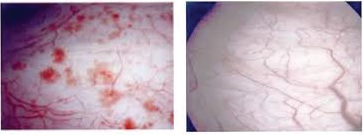
The diagnosis is not easy. Some features can be detected on cystoscopy (camera examination of the inside of the bladder) which may suggest the possibility.
How is the condition treated?
As the exact cause of the condition is not known for certain, no definite treatment is available. Simple things are attempted before moving to more complex and invasive lines of treatment.
Fluid advice
Avoiding inadequate fluid intake will avoid irritation of the bladder from concentrated urine. Avoiding excessive fluid intake will reduce distension of the bladder and thus pain before passing urine. Avoiding irritants, such as caffeine, alcohol, fizzy drinks, acidic drinks and smoking will reduce irritation of the bladder, and thus pain.
Stress management
Relaxation, listening to music, meditation and exercise may help.
Oral medication can help
Simple pain killers may be beneficial. The anti depressant Amitriptyline might be of value. Blood thinner Pentosan polysulfate sodium (Elmiron) could be used. Histamine receptor antagonist Cimetidine can be tried, knowing that it is not licensed.
Intravesical injections
A number of medications have been shown to help, including local anaesthetic Lidocaine, bladder wall covering Hyaluronic Acid, Botulinum toxin ‘A’, blood thinning Heparin, Dimethyl Sulfoxide and Chondroitin Sulfate.
The two commonly used injections locally include Hyacyst and Botulinum toxin ‘A’ (botox).
Hyacyst injections are made through a catheter inserted into the bladder.
This can be done in the Outpatient Clinic or through clean intermittent self catheterisation. Self administration avoids the need to attend at the hospital.
If you opt for self administration, you will be shown and helped to insert the catheter and introduce the Hyacyst yourself. Once you are comfortable doing this, you will be given the required injections and catheters.
You will be shown how to pass the catheter with the aid of a mirror. You will then be shown how to do this by sensation digitally (using your fingers) without having to use the mirror.
You should clean your hands each time before you insert the catheter. You need to prime the catheter, so that there is no air at the tip of the catheter.
You hold the catheter like a pen in your dominant hand and separate the labia with the other hand. You pass the catheter in and then inject the Hyacyst.
Several injections are often required before improvement can be noticed. A top up injection is made every few months, upon recurrence of symptoms.
Botulinum toxin ‘A’ (botox) bladder wall injection is made through cystoscopy (camera examination of the bladder). This is an operation that can be done under local or general anaesthesia. One injection is required, which may need to be repeated every few months.
For patients who do not improve on these measures, alternative treatments can be tried. Other measures that can be tried include electrical stimulation of bladder nerves. This can be done using the following:
- Leg nerve stimulation, using a hair thin wire. This can be done as an outpatient procedure and is known as Percutaneous Tibial Nerve Stimulation (PTNS). Twelve weekly sessions are required
- Trans-cutaneous electrical stimulation (TENS) machine, which is the same as the machine used in labour
- Sacral nerve stimulation. This requires the insertion of a wire into the back bone under general anaesthesia. A simulation battery is inserted above the hip bone
- Bladder distension with fluid
- Oral intake of cyclosporine A
- Cautery of bladder lesions
- Major surgery, like excision of the bladder and diversion of urine
Some of these measures require referral to other units.
Who can I contact with any concerns or questions?
If you have any problems or questions, you can contact:
Lewes Victoria Hospital Urogynaecology Unit
01273 474 153
Ext. 2178
Monday to Friday
9:00 am to 5:00 pm
Princess Royal Hospital Gynaecology Ward
01444 441 881
Ext. 5686
Royal Sussex County Hospital Gynaecology Ward
01273 696 955
Ext. 4013
Further sources of information:
The British Association of Urological Surgeons website
This patient information leaflet was prepared by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist
This information leaflet has been approved at the Clinical Governance and Safety and Quality Meetings of the Department of Obstetrics and Gynaecology as well as Brighton and Sussex University Hospitals NHS Trust Carer and Patient Information Group (CPIG).
Ratified April 2017 Women’s Safety and Quality Committee.
Disclaimer
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.