Download and print as a PDF (4MB pdf)
On this page
- Introduction
- What is the anterior cruciate ligament? (ACL)
- Tendon graft surgery
- After your operation
- Can I put weight on my knee?
- How long will I be in hospital?
- Getting home: Can I drive?
- How do I care for my wound and graft at home?
- What should I watch out for at home?
- Physiotherapy
- When can I return to sports?
- Exercises (weeks 1 to 2)
- Exercise Progressions
- Follow-up
- Contact Details
Introduction
This information is to help you with your recovery following the ACL reconstruction. It includes advice and exercises, and provides guidance about what to expect. The physiotherapy team and hospital staff will help you with your rehabilitation but it is important that you aid your recovery by:
- managing your pain and swelling
- doing your exercises regularly
- following the advice provided in this booklet.
What is the anterior cruciate ligament? (ACL)
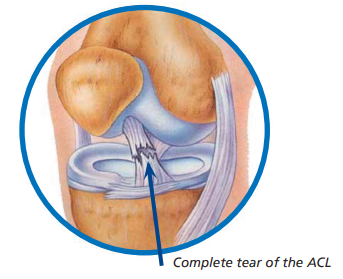
The knee joint is made of the femur (thigh bone), the tibia (shin bone) and the patella (knee cap). The knee also has ligaments that help to stabilise the joint. These include two collateral ligaments (on either side of your knee), and your PCL (posterior cruciate ligament) and ACL (anterior cruciate ligament) which cross each other inside your knee joint.
The ACL is a broad thick band which stops the shin bone from sliding forwards in relation to the thigh bone. It starts at the bottom of the thigh bone, passes down and forward, and attaches to the top of the shin bone.
The PCL is a strong thick band which stops the shin bone from sliding too far backwards in relation to the thigh bone. It starts at the back of the shin bone and attaches to the inside part of the thigh bone.
The most common causes of ACL injuries are:
- a direct blow to the knee
- a sudden deceleration, hyperextension (when the knee bends too far backwards) or rotational stress such as pivoting or landing from a jump.
Muscles also play a vital role in supporting the knee. These include the quadriceps or quads (front thigh muscles), hamstrings (back thigh muscles), and gastrocnemius (calf muscle).
Tendon graft surgery
The surgeon may use tissue from your own body to create a graft to reconstruct the ACL. This is called an autograft.
Most commonly this tissue comes from the hamstring tendons (back thigh muscles of your leg) or the patella tendon (the tendon that connects your knee cap to your shin bone).
If using a hamstring graft some tissue from the semitendinosus and / or the gracilis muscles is removed, and then carefully stitched together to make the graft. If using a patella graft the middle third of the tendon is removed.
Small tunnels are then drilled in the tibia and femur, and the graft is pulled through and secured in place. The graft is placed as close to the original ACL as possible and acts as a substitute for the damaged ACL.
Alternatively in some situations the surgeon may choose to use donor tissue. This is called an allograft. The surgeon will always discuss which option(s) he / she will use before your surgery and help you to decide which graft will give you the best possible outcome.
After your operation
Will I be in pain?
You may experience some pain and discomfort following your surgery. It is important that you inform medical / nursing staff if your pain relief is not working. When leaving hospital you will also be provided with painkillers to take home.
Will I have swelling?
Yes, it is normal to have swelling following surgery. However, excessive swelling will slow your recovery. It is therefore important that you do the following to reduce the amount of swelling in your knee:
• Rest regularly: do not walk or stand around for long periods (20 to 30 minutes). Complete rest is not advised either and you should aim for short periods of activity.
• Reduce swelling and aid pain relief by applying ice. We recommend using an ice pack for a maximum of 20 minutes and then taking it off for the rest of the hour. This can be repeated every hour as a maximum: you may use ice less frequently. Do not apply ice directly to your skin and do not get your dressing wet.
• Elevate your leg regularly throughout the day. This is particularly important in the first 72 hours and should be done whenever you are sitting down (unless you are doing your exercises).
Can I put weight on my knee?
Most people are allowed to fully weight bear but you will be informed by the physiotherapist if you are not allowed to put weight on the knee. This will vary depending on your surgeon’s preference. You will be in a knee brace or splint to limit the movement of your knee and we will give you crutches to aid your walking.
How long will I be in hospital?
Most people leave hospital one or two days after the operation. This gives you time to fully recover from the anaesthetic and have a session with the physiotherapist.
Getting home: Can I drive?
When leaving the hospital, you will not be able to drive and will therefore need to arrange your own transport or take public transport. If you take public transport, a responsible adult should accompany you home.
If you leave hospital on the same day as your operation, someone should stay with you for 24 hours after your surgery.
Be aware
You will not be able to drive until your consultant gives you permission to do so. If you drive before this your insurance will be invalid.
How do I care for my wound and graft at home?
The nurses will advise you how long you will need to keep your compression bandage on. If you have stitches and they need to be removed, they will give you advice about this. This can normally be done at your local GP surgery.
You should keep your wound dry and clean following surgery. We recommend a strip wash or, if you want to shower, sit down on a plastic stool while showering. It is essential you do not stand and slip on a wet surface as this could cause damage to the graft.
It is important that the wounds do not get wet as this can lead to infection. If you remove your brace or splint to wash it is essential that you hold the leg completely straight until it is reapplied.
The graft undergoes various changes once inside the knee. Please remember that the graft is weakest for 6 to 12 weeks after surgery so extra care should be taken during this time, especially in the shower.
What should I watch out for at home?
If you experience any of the signs below, please contact your GP or go to your nearest A&E department:
- your knee being more swollen or redder / hotter than normal
- new numbness, tingling or discolouration in your foot
- temperature above 37°C
- oozing wound
- persistent calf pain or swelling.
Physiotherapy
Movements to avoid
The following movements put a strain on the graft and therefore need to be avoided until advised by your outpatient physiotherapist or consultant:
- Twisting, pivoting or turning abruptly on the operated leg.

Brace
Before you go home, a physiotherapist may fit you with a brace like the one below if this is required.
Once fitted, the brace is easily put on and taken off simply by opening the Velcro straps and then the foam pads underneath. When removing the brace for hygiene purposes your leg should be held straight until you put the brace back on.
The physiotherapist will lock the brace with the range of movement specified. You should not alter this range of movement setting unless advised to by a physiotherapist or surgeon. The
brace should be worn 24 hours a day and only removed for washing and dressing purposes. You must continue to wear this brace until you are advised to remove it by your physiotherapist
or surgeon. This is likely to be a minimum of 2 weeks.
If the brace gets dirty it can be washed with soap and water and left to air dry.
The physiotherapist will also run through your exercises and teach you how to walk with crutches. Once confident on your crutches, you will be shown how to go up and down the stairs. You should remain on your crutches until advised by your consultant or outpatient physiotherapist.

The physiotherapist will also run through some ways in which you might need to modify your daily routine.
When can I return to sports?
It is important that you do not return to sport too early because this can result in re-injury and failure of the surgery. Your consultant and outpatient physiotherapist will advise how and when you can start training for sport again.
At 4 weeks you are allowed to return to swimming (excluding breast stroke/ frog leg kicks) as guided by your physiotherapist. You should not return to pivoting sports until 12 months after
surgery and should only return to competition after discussion with your physiotherapist or surgeon.
Exercises (weeks 1 to 2)
It is important that you start these exercises immediately and find time to do them at least three to five times a day. You must do only these exercises (do not add your own), until you are progressed by the outpatient physiotherapist. These exercises should not cause excessive pain. If you have any concerns about a particular exercise causing pain then stop doing that exercise and contact the physiotherapy department for advice.
- Ankle pumps: to help prevent a deep vein thrombosis (DVT) it is important that you maintain good circulation in your lower legs. Push your foot down and away from you (point toes). Then bring your toes up towards your shins (flex your ankles). Repeat 10 times, 5 times per hour. Continue this exercise for the next 3 days.

- Calf stretch: sit up in the bed with your legs out in front of you. Put a towel around your foot. Gently pull your ankle towards you and feel the stretch in your calf. Hold for 30 seconds. Repeat 3 times in a row.

- Static quads: sit or lie with your leg straight and then contract / tighten your quads (front thigh muscles) as hard as you can by pushing your knee downwards. Hold for 5 seconds and then relax. Repeat 10 times.
- Knee flexion in lying: lying on your back. Slowly bend and straighten your operated leg: ensure the movement is controlled and that your foot maintains contact with the bed at all times. Bend your knee as far as is comfortable or as far as your brace allows. Repeat 10 times.

- Co-contractions: lying on your back. Place a small towel roll under your operated knee. Push your heel down into the bed to activate your hamstring muscles. At the same time push the back of your knee onto the towel roll to tighten your quadriceps muscle. Hold for 5 to 10 seconds and then relax. Repeat 10 times.

- Knee cap mobilisations: lie or sit with your leg straight and relaxed. Gently move your knee cap from side to side with your fingers as shown in the picture. Repeat 10 times.

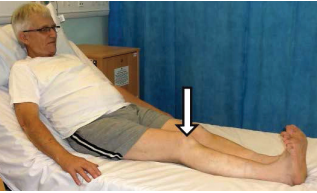
- Straight leg raise: lying on your back with your leg straight. Pull your ankle up towards you, push your knee down and then raise your operated leg about 15cm off the bed. Ensure the knee stays straight. Hold for 5 seconds. Repeat 10 times.

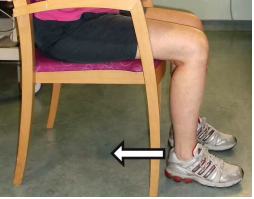
- Knee flexion in sitting: sit on a chair with your feet on the floor. Bend your knee as far as is comfortable or as far as your brace will allow. Then straighten your leg. Repeat 10 times.
- Extension stretch: Sitting on a chair, with your operated leg supported as shown. Relax and let the knee straighten with gravity. Stay in this position for 2 to 5 minutes. You can also do this exercise lying down on your bed: place a rolled up towel underneath your heel and then relax your leg.

- Hamstring stretch: sit on a chair with your operated leg straight and your heel resting on the floor. Lean forwards keeping your back straight until you feel a stretch along the back of your leg. This exercise can also be done sitting in bed. Stretch your operated leg out in front of you and reach forwards towards your toes. Hold for 30 seconds.

- Hamstring curl: stand and hold on to a stable surface. Bend your operated knee to lift your foot slowly off the floor. Bend your knee as far as is comfortable or as far as your brace will allow. Slowly lower the foot back down. Repeat 10 times.

Exercise Progressions
You may progress to these exercises at two weeks post-surgery as advised by your physiotherapist.
- Seated knee extension: sit in a chair with your foot flat on the floor. Lift your foot off the floor and straighten your knee. Repeat 10 times.

- Single leg standing: only begin this exercise when your pain is adequately controlled and you can weight bear well through your operated leg. Stand and hold on to a stable surface. Stand on your operated leg and lift your other leg off the floor. Hold for 10 seconds and repeat 10 times. Slowly lower the foot back down. Gradually increase the time to 30 seconds and begin to reduce the amount of support on your arms.

Follow-up
Physiotherapy
You will be seen by an outpatient physiotherapist at your local physiotherapy department approximately two weeks after leaving hospital. He / she will check your range of movement and exercises to ensure that you have the correct technique. You will also receive a new exercise programme.
If you do not receive an appointment for outpatient physiotherapy after 1 week of leaving hospital then please contact your local physiotherapy department, if they are unable to help then please call the inpatient physiotherapy department to assist you.
GP
You may need to visit your GP 10 to 14 days after your surgery for a wound check. The nurse will advise you about this on discharge.
Orthopaedic surgeon
An appointment with your surgeon will normally be arranged for you two to three weeks after your surgery.
Contact Details
Inpatient Physiotherapy Team
0333 200 1728
Ext. 68834
Newick Ward
0333 200 1728
Ext. 68829
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no wayintended to replace professional clinical advice by a qualified practitioner.