Download and print as a PDF (225kB pdf)
On this page
This leaflet is intended to answer some of the questions of parents or carers of children diagnosed with Myopia under the care of University Hospitals Sussex NHS Foundation Trust.
What is Myopia?
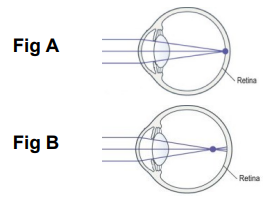
When no glasses are required the image of what you are looking at is focussed sharply on the retina at the back of the eye (Fig A picture below). Myopia is often the result of the eyeball being too long, meaning the eye does not focus light sharply on the retina at the back of the eye. In myopia the light is focussed at a point in front of the retina (Fig B picture below), making the light that actually falls on the retina blurred. A child with mild myopia is likely to see things close up better than further away. For this reason myopia is also known as near-sightedness or short-sight.
What causes myopia?
There is usually no particular cause of myopia. Sometimes the child’s parents have myopia and so it is inherited. Some other genetic conditions may mean a child is more likely to develop myopia.
What are the signs and symptoms?
It is not uncommon for children to show no signs of myopia in the first years of life and it is typically only diagnosed when children are between 7 and 11 years old although it can occur at any age.
Children are good at adapting to blurred vision and will often not show any signs of having myopia. Sometimes a child can want to sit closer to the TV than normal, or complain of headaches and blurred vision.
How will you test the vision?
Vision tests are available for all age groups, ranging from pictures that are simply looked at, to matching pictures or letters on a card, to naming letters or numbers.
How do you know my child needs glasses?
This is done by an Optometrist. Young children are often asked to have eye-drops put into both eyes before the optometrists appointment. These eye drops limit the ability to focus for a few hours so that the optometrist can get an accurate reading. The eye drops also widen the pupils to give the optometrist a good view of the back of the eye.
Can it be treated?
Glasses or contact lenses can be used to make the vision clearer. Glasses are the most common method used in children. The lenses used to correct myopia are called ‘concave’ or ‘minus’ lenses and are indicated by a minus sign on the glasses prescription.
Unless told otherwise by your orthoptist or optometrist the glasses are to be worn all of the time.
Children’s vision usually improves gradually and this can take up to 18 weeks to fully adapt to the glasses.
Are there associated complications?
Sometimes the low vision associated with myopia can cause a strabismus. Strabismus is the term used to describe eyes that are not pointing in the same direction and not working together.
The type of strabismus seen in someone who has myopia is commonly an exotropia. This is when the eye turns outwards away from their nose.
This can be managed with glasses and / or an operation. This condition is not very common.
Another complication can be amblyopia (reduced vision in one eye). This can occur if the glasses prescription is higher in one eye than the other.
Amblyopia can resolve over time as glasses are worn.
If it persists, despite good compliance with glasses, then occasionally we need to do some patching treatment.
This involves wearing an eye patch over the better seeing eye for a few hours per day to help encourage the vision to develop.
Your Orthoptist will advise you if this is necessary.
Will my child need glasses for the rest of their life?
The most likely answer is yes. As children grow their prescription will change but in myopia it is more common for the prescription to increase rather than decrease. Myopic children will likely wear glasses or contact lenses long term.
Contact Details
St Richard’s Hospital
St Richard’s Hospital
Spitalfield Lane
Chichester
West Sussex
PO19 6SE
Orthoptist
01243 831499
Southlands Hospital
Southlands Hospital
Upper Shoreham Road
Shoreham-by-Sea
West Sussex
BN43 6TQ
Orthoptist
01273 446077
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.