Download and print as a PDF (508kB pdf)
On this page
- Why is this procedure performed?
- How is the procedure performed?
- What are the benefits?
- What are the risks?
- Frequently asked questions
- What happens after the operation?
- When and how do I have the stitches removed?
- Will I have to use eye drops after the operation?
- Will I be able to see it straight away?
- When can I resume normal activities?
- What if I have any problems or worries?
The cornea is the clear window at the front of your eye, through which light rays pass onto the back of the eye or the retina. To be able to see clearly, your cornea must remain transparent, healthy and in the correct shape.
The cornea has several layers from front to back, and the innermost layer is called the Descemet membrane. This membrane has endothelial cells responsible for pumping fluid out of the cornea. These cells cannot regenerate. So when the endothelial cell count is reduced, the cornea can swell up and become hazy, affecting your vision. In severe and long-standing cases, this condition can also be painful. The only way to treat that is to replace the diseased layer with a transplant surgically.
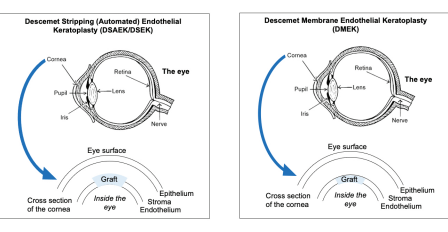
• Descemet’s membrane endothelial keratoplasty (DMEK) is a procedure where the inside or back layer of the cornea, known as the Descemet membrane, is removed and replaced with a similar layer from a donor cornea. This layer is fragile, represents 10% or less of your total cornea, and carries endothelial cells.
• Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) is a similar procedure; however, a thicker back layer of the cornea is used, which also has other corneal tissue (stroma) along with the Descemet membrane. An automated machine often prepares this in the eye bank.
Why is this procedure performed?
The procedure is performed to improve one’s vision when the poor function of the inner endothelial cell layer has led to corneal water logging or oedema. The most typical indication is Fuchs corneal dystrophy. DMEK is now the preferred procedure; however, in certain circumstances, or if the cornea is very hazy, your surgeon may offer you DSAEK.
How is the procedure performed?
If you have a cataract, you can simultaneously have DMEK and a cataract operation. Both procedures take about 90 minutes and are often performed under local anaesthetic. However, this may vary, and you can discuss more with your doctor. During the operation, the dysfunctional innermost layer of the cornea is removed and replaced by similar tissue specially prepared from a donor cornea. Only a small opening in the eye’s surface is required for this procedure. The graft is held in place using a bubble of gas or air. Small stitches seal the wound to prevent gas escape; otherwise, the graft can detach or come off.
What are the benefits?
This surgery aims to improve your vision. Your vision should improve much quicker than if a full thickness graft was used.
What are the risks?
The risks of the surgery include, but are not limited to:
• Infection.
• Bleeding.
• Graft rejection, detachment or displacement.
• Glaucoma.
• Damage or inflammation to the back of the eye (retina).
• Need for further procedures.
• Loss of vision (1 in 1000).
This operation is usually carried out under local or general anaesthesia. There can be risks associated with the anaesthesia used. For further information about the risks of anaesthetics, please see the booklet ‘You and your Anaesthetic’ or visit The Royal College of Anaesthetists website
Frequently asked questions
Are there any alternatives to this surgery? Penetrating keratoplasty is an alternative to this procedure. This involves a full thickness graft.
What happens if I opt not to have the surgery? If you have been offered the surgery, your corneal endothelial cells are not functioning correctly. This condition will progress with time, though the rate can vary.
What happens now I am on the waiting list? There will be other people on the list ahead of you, and you will have to wait for donor eye material to be available. This period can vary.
When donor material has been arranged, you will usually be given a few weeks’ notice by post (and / or telephone) of your admission date, though sometimes this may be only days (in case of cancellation replacements).
What happens after the operation?
• You may remain admitted to the ward for the first night of your surgery. Your surgeon will review one to two hours after the surgery on the day and the next morning.
• If your graft does become detached or displaced, you may require additional rebubbling. This can either be done in the theatre or clinic. A very small amount of air or gas will be injected into the eye under an appropriate anaesthetic cover.
• Although strict positioning is unnecessary, you may be asked to lie flat on your back after the operation for the first two to three days.
• The air or gas used to hold the graft in place will gradually be absorbed in the days after your operation.
• You may experience some pain in your eye after the operation. However, this should settle with paracetamol. If your pain does not settle, please seek help.
When and how do I have the stitches removed?
Stitches will be removed in the clinic within a few weeks.
Will I have to use eye drops after the operation?
Yes. You will be given steroid drops to help prevent graft rejection. These will be provided along with clear instructions when you are discharged. Initially, you will have to use these drops every few hours and then gradually reduce in frequency over months.
Long term, you will be advised to continue drops (once or twice a day) for at least one to two years and may be longer, depending on your clinical situation. You will be regularly followed up in the outpatient clinic after the surgery, and your doctor will advise you regarding stopping drops when appropriate.
Will I be able to see it straight away?
Your vision is expected to be blurred for a few days but should start to improve gradually over the first couple of months. You are likely to require glasses after the operation. You can get these from your regular opticians.
When can I resume normal activities?
• Work: You are likely to need one week, or longer, off work, depending on the type of job you have.
• Sport / hobbies: We advise waiting for four weeks before returning to sports or active hobbies.
• Flying: Air travel is not safe until the gas bubble is in your eye, which may be up to 2 weeks. Please confirm with your doctor on a follow-up visit if you can fly.
• Driving: You should avoid driving after the operation. We recommend waiting a few weeks before driving, allowing your vision to improve.
What if I have any problems or worries?
After the operation, it is important to contact the hospital immediately if the eye becomes sore, red, light-sensitive, or blurred vision. This could represent a rejection of the graft and requires urgent treatment.
Contact details
If you have problems or need urgent advice, ring the eye hospital. Ask for the Accident and Emergency Department (A&E) or Nursing Staff. There is always someone on duty, night and day.
Sussex Eye Hospital
Eastern Road
Brighton BN2 5BF
Out of hours
01273 664881
Compiled by Ms Ritika Mukhija, MBBS, MD, FRCOphth, Dr Gabriella Quiney and MBBS, Mr Mayank A. Nanavaty, MBBS, DO, FRCOphth, PhD.
This leaflet is intended for patients receiving care in Brighton and Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.