Download and print as a PDF (271kB pdf)
On this page
What is Necrotising Enterocolitis (NEC)?
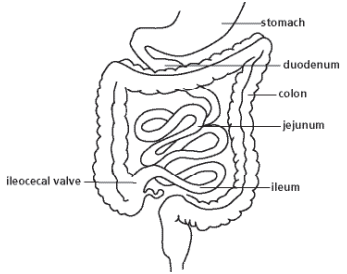
Necrotising Enterocolitis is a condition that generally affects premature or low birth weight babies. It usually involves the terminal ileum (last part of the small intestine) and the colon (large intestine), but can affect any part of the bowel (gut) from the stomach to the rectum. NEC is a serious condition which is usually treated medically but may need surgery and can in some cases be life-threatening.
What causes NEC?
No single cause has been found for NEC but it is thought to be the result of a combination of different things. Babies born early can have this problem. The premature intestines can be sensitive and the gut may not fully digest the milk feed. In severe cases the intestine may be badly affected and part of it may need surgical removal.
What are the signs and symptoms?
Your baby may be quiet, lethargic and not tolerating feeds. Your baby may have large aspirates (a lot of milk is still found in the tummy at the next feed), bilious vomiting (greenish in colour), have a distended abdomen (swollen tummy) or bloody stool (poo). If any of these signs are found by the nurses they will inform the doctors and ask them to examine the baby. When the doctor examines your baby they may show signs of some discomfort and their tummy may look darker around the umbilicus (belly button).
How is NEC diagnosed?
Diagnosis can be difficult and a collection of all the signs will be used to suggest a diagnosis. Often babies are treated for suspected NEC before a clear diagnosis is made as waiting could result in the gut wall getting worse. The gut may become very swollen and weak allowing a hole to develop. This is called a perforation. X-rays of the abdomen can help in diagnosis and look for perforation.
What is the treatment for NEC?
NEC is treated by stopping baby’s feeds. This helps bowel swelling disappear. Your baby will also be treated with intravenous (drip in the vein) antibiotics which will continue for 5 to14 days. Your baby remains Nil by Mouth, without feeds, for between 5 to14 days, this is to allow enough time for the bowel to recover. The nasogastric tube – the tube in their nose/mouth down into their tummy – will be put on what’s called ‘free drainage’. This means the end will be opened to let any stomach contents drain out into a drainage bag.
As your baby may not be fed milk for up to 14 days they will need to be given a drip called TPN (Total Parenteral Nutrition). This provides all the nutrients they need to recover and grow. Once milk feeds begins again the TPN will be decreased as your baby’s tummy is able to have more milk. Regular blood tests will be taken and your baby may need to have blood or platelet (blood cells that control bleeding) transfusions, as these need topping up in NEC.
The doctors will inform the surgeons of your baby’s condition and if they think it necessary, they will visit your baby. When feeding begins it is felt best to feed your baby on Expressed Breast Milk (EBM). The nurses will talk to you about expressing and storing your milk during this time. If you are unable to express, the nurses will discuss with the doctors the use of Donor EBM or formula to see which would be best for your baby.
Will an operation be needed?
Surgery may be needed if the intestines do not respond to treatment or if the intestine has a small hole in it. The surgeon will have seen your baby and will need to talk about the operation with you. The surgeon will explain the procedure and what they expect to find. They will ask you to read and sign a consent form. The operation is performed here at the Royal Alexandra Children’s Hospital. An anaesthetist will care for your baby during the operation. Your baby will have a general anaesthetic and be asleep throughout the operation; your baby will feel no pain or discomfort.
Surgery may involve removing the part of the intestine if it is damaged. The surgeon will try to remove as little intestine as possible and to join the ends back together. However, it may be necessary for your baby to have a stoma (small opening) formed. This is where the healthy intestine is brought up to the skin surface and a pouch is attached to collect the stool (poo). This gives the intestine a chance to recover before the ends are joined back together.
If a stoma is needed the Stoma Care Nurses will come up to the unit to meet you and your baby. They will provide help with stoma pouches and care of the stoma.
Following surgery your baby will remain on a ventilator to allow them to recover safely. The doctors and nurses will give pain relieving medicines for as long as needed. This will probably start as a drip containing Morphine and then be reduced to less strong pain killers, such as Paracetamol over time.
When will feeding start again?
Once the surgeons and doctors are happy with the bowels recovery, small amounts of milk are introduced again through the nasogastric tube. The amount will be increased slowly as so that your baby’s tummy gets used to it. As the milk amount increases the intravenous TPN will be decreased and then eventually stopped.
What is the final outcome?
When NEC is treated medically by resting the bowel, the outlook is good with most children growing up to lead normal lives. For children that have had surgery the outcome depends on the amount of bowel removed and how prematurely your baby was born. If a large amount of bowel was affected your baby may need to stay on TPN for a longer period of time to allow them to grow and until your baby’s the bowel is able to cope with normal feeds again.
What about follow up?
If treated medically your baby will be followed up in Neonatal Outpatients as usual. If surgery was needed, your baby may also have a Surgical Outpatients appointment.
Where can I get additional support?
You can talk to the doctors and nurses treating your baby for additional information. If you need an interpreter the nurses can arrange for one to be present. Interpreters for the deaf or hard of hearing are also available on request. If you would like to seek support from the counsellor attached to the unit do let the staff know.
There is no specific support group for NEC but parents may find it helpful to contact Bliss which is a premature baby support group. Their website is www.bliss.org.uk
References
www.pedisurg.com – diagrams
Who should I ask if I have any further questions?
The nurse and neonatal team looking after your baby will be happy to answer any further questions you may have.
Trevor Mann Baby Unit
The Royal Sussex County Hospital
Eastern Road
Brighton BN2 5BE
TMBU
01273 696955
Ext. 6437
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.